Coronavirus is a family of enveloped RNA viruses that include the original SARS coronavirus (SARS-CoV) and the recently emerged SARS-CoV-2. According to the World Health Organization, there have been over 500 million confirmed SARS-CoV-2 infections, and well over 6 million deaths from coronavirus disease 2019 (COVID-19).1 Although the recovery rate from COVID-19 is estimated to be closer to 98%, many of the ‘recovered’ patients, in general, and those who were hospitalized, in particular, may not recover completely. Emerging reports indicate that SARS-CoV-2 induces a storm of inflammatory cytokines, including interleukins and adhesion molecules, that can induce severe airway inflammation.2 Although the airway inflammation subsides in the majority of patients with COVID-19, a cohort of patients known as ‘long-haulers’ suffer from a myriad of persistent symptoms, including fatigue, dyspnoea, myocarditis, hypertension and severe lung damage that culminates in respiratory dysfunction.3–5
To date, the underlying molecular mechanism(s) for the respiratory dysfunction seen in patients with long COVID has not been completely characterized. It is also not known what proportion of these patients may develop lung fibrosis because of SARS-CoV-2 infection and delayed recovery from COVID-19 complications. This is in part because of the relatively short time since the start of the pandemic and the resulting lack of long-term follow-up studies, including repeated lung function tests and chest computed tomography (CT) scans to evaluate the presence and progression of lung fibrosis. However, animal models and lung biopsies from deceased patients with COVID-19 provide a snapshot of the extent of lung damage and profibrotic changes that result from the viral infection.6,7
Preclinically, several animal models, including mice, rats, hamsters, ferrets and monkeys, have been studied to mimic aspects of the pathogenesis of the SARS-CoV-2 infection. Although there is no gold standard animal model that can completely mimic the pathogenesis of SARS-CoV-2 infection in humans, the Syrian hamster model has been able to manifest several features that resemble the lung pathology seen in cadaver lungs from patients with COVID-19. The infected animals show rapid breathing within 1-week post-infection, and histopathological studies of the explanted lungs demonstrate high viral load, interstitial pneumonia, immune cell infiltration, diffuse inflammation, severe haemorrhage, large areas of consolidation, alveolar destruction and fibrosis.8–10 Similarly, large-animal models including non-human primates, show inflammation, diffuse alveolar damage and ground-glass opacities (GGO) in response to SARS-CoV-2 infection.6
Clinically, lung autopsies from deceased patients with COVID-19 show signs of profibrotic disease, including aberrant activation of pro-inflammatory macrophages and endothelial cells, failed regeneration of epithelial cells, overproliferation of fibroblasts and differentiation into collagen-synthesizing myofibroblasts.11,12 Histopathological studies revealed that lung tissues from patients with COVID-19 with longer duration of illness (up to 47 days from the onset of symptoms) show diffuse interstitial fibrosis and high expression of profibrotic markers such as collagen 1 and alpha smooth muscle actin.13 In general, there is a negative correlation between SARS-CoV-2 viral load and processes that support respiratory function, including surfactants and the basal cell population. Antemortem plasma samples from patients with COVID-19 also showed that the levels of lung repair-related proteins such as fibroblast growth factor 2 and stem cell factor are significantly depleted in comparison with the plasma levels in uninfected individuals.13 By contrast, patients with COVID-19 were found to have elevated levels of fibro-inflammatory proteins such as tumour necrosis factor alpha, interleukins (e.g. IL-6), macrophage chemotactic proteins, growth factors, transforming growth factor beta, and cell death-related proteins such as caspase 8 and the natural cytotoxic receptor 1.13–15
A systematic review that compiled 45 chest CT scan-based studies of over 4,000 patients with COVID-19 reported that GGO with or without consolidation was the most common lesion observed, affecting over 40% of the patients. Additional pathological findings include pulmonary vascular enlargement, intralobular and interlobular septal thickening, pleural thickening and bronchiectasis. When GGOs failed to resolve, they increased in size, number and density and progressed into fibrosis.16 It also appears that there is a positive correlation between the severity of lung damage, age at infection and the duration of illness.16,17
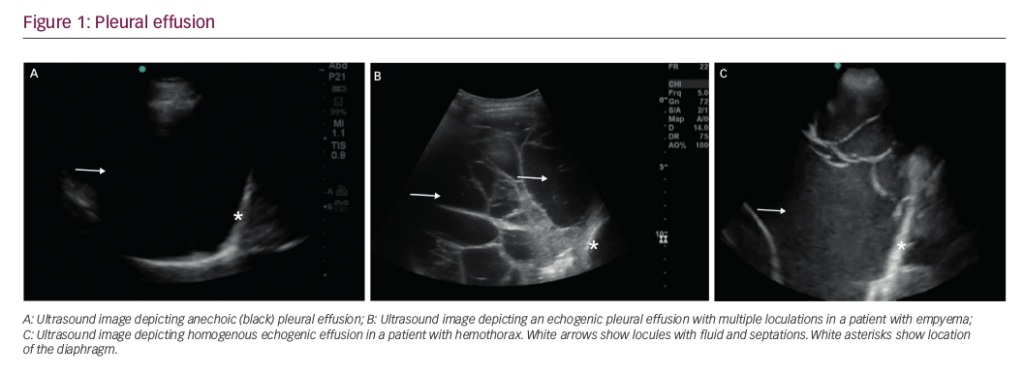
More recent prospective studies indicate that a proportion of patients with COVID-19 experience fibrotic lung remodelling and decreased exercise tolerance about 1 year after hospitalization from SARS-CoV-2 infection.18 A longitudinal study of 83 patients with COVID-19 treated at the Wuhan University Hospital observed that significant abnormalities in lung function, such as a reduction in the diffusing capacity of the lungs for carbon monoxide, remained after 12 months. Radiological abnormalities such as GGO, interstitial thickening and reticular opacity were also evident in 24% of the patients 12 months after discharge. However, there was no evidence of progressive interstitial abnormalities, including fibrosis, during the follow-up period.18 Another study of 46 patients with COVID-19 who tested negative for SARS-CoV-2 by reverse transcription polymerase chain reaction showed that most of the patients had multiple pulmonary lesions, including GGO, pleural effusion, vascular enlargement, bronchiectasis and interstitial thickening.19 More worrisome is the diagnosis of pulmonary fibrosis in 56% of the patients who had moderate disease, and in 71% of the patients who had severe COVID-19 only 3 months after recovery.19,20 Similar findings were reported in study of 130 patients with COVID-19, where 40.8% of symptomatic patients (n=53) showed evidence of lung fibrosis on CT scans.21
While we wait for long-term studies on the respiratory complications of COVID-19, including the development and progression of lung fibrosis, it is important to revisit the literature on respiratory abnormalities caused by the original SARS-CoV. A follow-up study of 110 SARS survivors reported that 30% had abnormal chest radiographs and impaired lung physiology, including decreased exercise tolerance 6 months after the onset of symptoms.22 Notably, the patients who required intensive support during active infection had a greater risk of developing lung fibrosis than those who were treated in the general wards.22 An observational cohort study that followed 71 patients with SARS for 15 years reported that 4.6% of the patients had persistent pulmonary lesions, including GGO, on CT scans. However, interstitial abnormalities were mostly reversed or stabilized within 2 years of rehabilitative therapy.23 In this regard, similarities and differences in the pulmonary structure and function caused by the two coronaviruses need to be reviewed to inform the current standard of care for patients with COVID-19.
Conclusion
Preclinical and clinical studies indicate that SARS-CoV-2 infection results in high lung viral loads and culminates in severe lung damage characterized by impaired regeneration and the build-up of abnormal extracellular matrix components, including collagen. Although it is premature to predict what proportion of patients with COVID-19 may end up developing lung fibrosis, it is plausible to hypothesize that elderly individual and patients with underlying chronic diseases are likely to be disproportionally affected. Although vaccine is the primary preventative strategy to inhibit infection or the development of severe disease when infected, antiviral agents, anti-cytokine therapy and antifibrotic drugs should also be empirically tested and developed for the prevention and/or treatment of SARS-CoV-2 infection and long-term health complications, including respiratory failure. In societies where these preventative and therapeutic strategies are not in place or when people fail to comply with public health measures to mitigate COVID-19 infection, we may see an increasing number of infected patients developing severe and chronic complications such as pulmonary fibrosis. Unfortunately, there is no treatment that can halt or reverse lung fibrosis. Once developed, lung fibrosis is a dismal disease that relentlessly destroys many vital structures, including the alveoli, interstitium, airspaces and the pulmonary vasculature, resulting in dyspnoea and death within 3 to 4 years of diagnosis.