Inducible laryngeal obstruction (ILO), previously designated as vocal cord dysfunction (VCD), is characterised by a transient and reversible narrowing of the larynx in response to external triggers, resulting in symptoms such as cough, dyspnoea and noisy breathing.1,2 Adduction of the vocal folds usually occurs in inhalation but can also happen in exhalation, restricting movement of breath through the glottis airway.3 The terminology used to describe ILO was vast, besides VCD, terms like paradoxical vocal fold motion and paradoxical vocal cord motion have been used. In 2013 a nomenclature for ILOs causing breathing problems was proposed by Christensen et al. on behalf of the European Respiratory Society, the European Laryngological Society, and the American College of Chest Physicians task force on ILOs, establishing the term ILO.2
ILO has gained greater recognition in the past two decades, but the first description was by Dunglison et al., in 1842, who described it as “hysteric croup”.4 In 1983, the term “vocal cord dysfunction” was used by Christopher et al. to describe a distinct clinical entity, a syndrome of vocal cord adduction with a posterior chink presenting as asthma in five patients with ILO and a history of uncontrollable asthma.5
The aim of this article is to summarise current understanding and provide a review of the literature of ILO in the paediatric population. PubMed searches were performed for articles published using combinations of the keywords: vocal cord dysfunction, paediatrics, ILO, and exercise ILO. The articles were selected based on their relevance to the topic of this review.
Epidemiology
The prevalence of ILO in general adult or paediatric populations is uncertain,1 given the fact that most of the data have been reported in the context of case reports or occasionally case series. A review of the literature on the reported causative factors and treatments for VCD by Morris et al., found that 29% of the patients with VCD were within the paediatric age, and the average age of diagnosis in the group was 14.5 years.6 Brugman identified 35% of the VCD reported cases were children with a median age of 14 years.7 ILO is more common in females, with a 2:1–3:1 predominance.8–10
ILO can cause exercise-induced symptoms and be misdiagnosed as exercise-induced asthma, unresponsive to treatment.1 Seear et al. diagnosed VCD in 27% of school children referred for investigation of poorly controlled exercise-induced asthma, based on clinical symptoms, flow-volume loops and negative exercise treadmill test results.11 A Boston Children’s Hospital study, where 294 patients were evaluated for exercise-induced dyspnoea, identified 29.7% of the patients as having VCD, diagnosed by laryngoscopy.12 Another study by Johansson et al. reported that exercise-induced laryngeal obstruction (EILO) was present in 10.8% of adolescents with exercise-induced dyspnoea, estimating the prevalence of EILO in the population was 5.7%.13
ILO has also been reported in newborns. Omland and Brondbo described a case series of four infants that presented stridor since birth, and laryngoscopy showed a paradoxical vocal cord movement with adduction of the vocal cords during inspiration in all of them.14 However, in this age group, there are other confounding factors such as laryngomalacia that should be taken into account, making it more difficult to identify ILO in such young age.14
Pathophysiology of inducible laryngeal obstruction
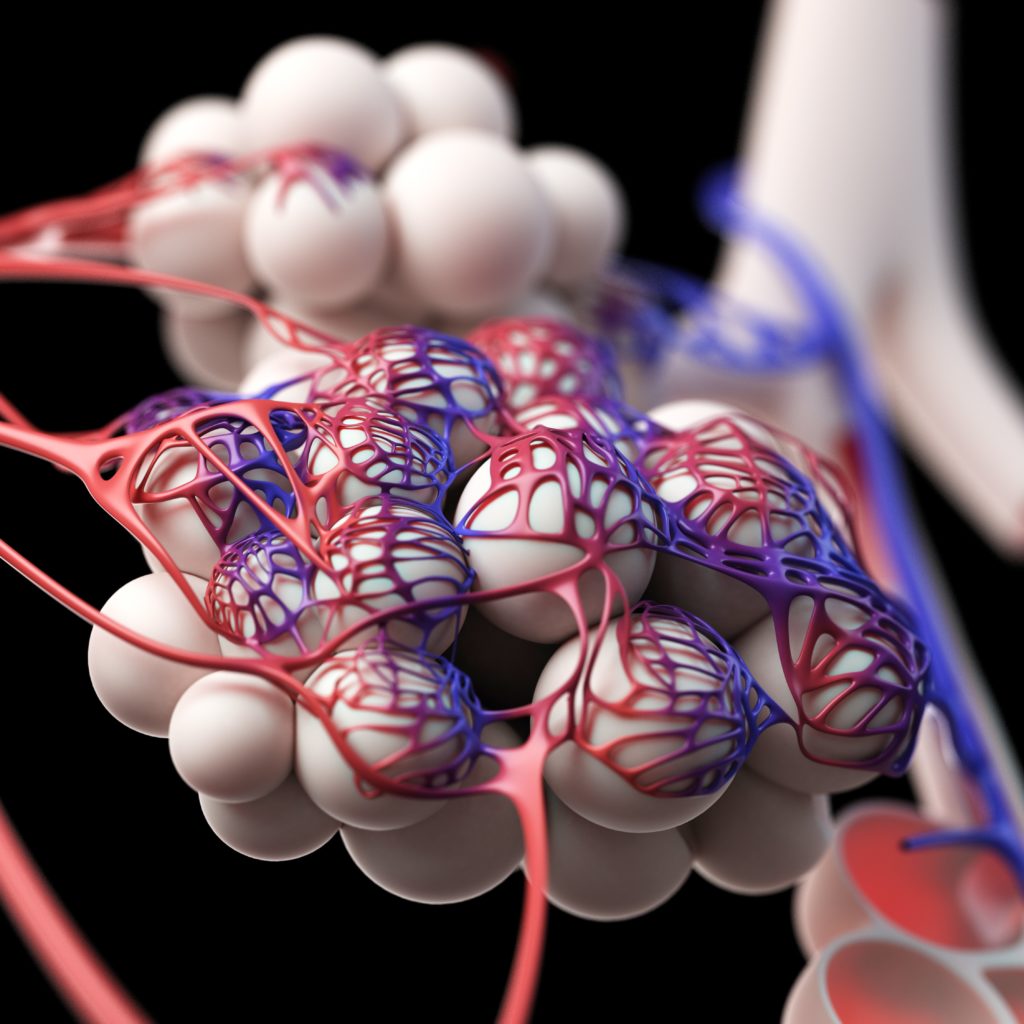
ILO is a complex entity and the exact mechanisms are still unclear; it cannot be explained by a single pathophysiological mechanism.10,15,16 The larynx provides complex muscular and centrally mediated neural mechanisms regarding the coordination of critical functions like breathing. The glottic closure reflex is a protective function that prevents deleterious inhalants from entering the trachea and lungs.15 Reflex-associated ILO may be explained by direct stimulation of sensory nerve endings, which in turn could induce a protective reflex, triggering laryngeal closure and protecting the airway from aspiration or asphyxiation.16
There are reports of nonorganic and organic causes of ILO in current literature.17 Nonorganic refers to psychological factors, such as conversion disorder, depression, obsessive-compulsive and anxiety disorder.9,18 A previous history of sexual abuse could also be associated with ILO. Freedman et al. described three cases of paradoxical VCD in women, initially diagnosed with intractable asthma, and who had been victims of sexual abuse in childhood.19
ILO in paediatric populations, including small children, may have multiple possible aetiologies, with some precipitating factors as known triggers. These triggers can include psychological and emotional disorders/stress, extreme temperatures, physical exercise, extrinsic (chemical, sensory, and gastroesophageal reflux) and intrinsic airway irritant (laryngopharyngeal reflux or rhinitis/sinusitis, chronic allergic or non-allergic rhinitis with post nasal drainage).3,8,9,18 Evidence shows that a high level of organised sport practice is common in paediatric patients with ILO.8,20,21 The frequency of concomitant asthma and reflux symptoms in these patients supports the theory that laryngeal hypersensitivity may be a significant factor in the pathophysiology of ILO.20
Gastroesophageal reflux may cause direct damage to the laryngeal mucosa, leading to ILO when it causes laryngopharyngeal reflux.8,15,16,18 The laryngeal mucosa seems to be more sensitive to acid reflux than the oesophagus and stomach mucosa, making it more susceptible to the damage caused by the reflux, resulting in an exacerbation of the glottis closure reflex.9 Approximately 18% of all patients with ILO are reported to have gastroesophageal reflux disease (GERD).6 In the paediatric population, the relationship between GERD and ILO is stronger, and several studies have identified GERD history in patients with ILO;6,21,22 36–95% of the children exhibit clinical laryngeal signs of laryngopharyngeal reflux.23
Another trigger for ILO is postnasal drip secondary to common conditions in the paediatric population, such as allergic rhinitis, sinusitis and upper respiratory tract infection, that cause an inflammatory insult.8,18 Taramarcaz et al. suggested that viral infections cause epithelial damage, which leads to inflammation in the larynx and extrathoracic airways. In these cases, the ILO appears to be transitory, with total recovery after acute viral infection.24 Other exposures, such as smoke, fumes, vapours, perfumed products, air pollutants and chemical agents can also induce ILO symptoms.8,16
In the newborn cases described by Omland and Brondbo, the mechanism involved in ILO may be the expression of immaturity in the neural balance between the laryngeal sphincter and respiratory function.14
ILO can be associated with psychiatric disorders. In 1998, Gavin et al. found higher levels of anxiety and anxiety-related diagnoses in children with VCD compared with asthma patients,25 and in 2011 Mutaro et al. reported that 30.5% of the patients diagnosed with VCD had an underlying psychiatric condition.26 More recent studies have revealed that psychological issues may not be present as frequently as initially assumed; Smith et al. did not find any associated psychiatric diagnoses in the studied patients.20
Inducible laryngeal obstruction and asthma
As previously mentioned, ILO can mimic asthma, but asthma is more than a differential diagnosis of ILO, as these two pathologies can coexist in the same patient in 35–60% of adult patients.9 Literature regarding simultaneous diagnosis of ILO and asthma predominantly include the adult population. Newman et al. identified 56% of adult patients with laryngoscopically proved VCD as having both pathologies, based on reactive bronchoprovocation testing or positive bronchodilator response.27 Another adult population study reported coexistent asthma in 35% of the patients with VCD, based on the same parameters.28
Traister et al. found in a retrospective study that 63% of adult patients with VCD had, at some time, been given a wrong diagnosis of asthma, and had been misdiagnosed with asthma for 9 years.29 In the Newman et al. series, more than 75% of the patients without asthma were receiving a mean of 29 mg of prednisolone daily, for more than 4 years.27 Kramer et al. also reported high use of asthma treatments in adults with VCD, with 85% of the patients taking asthma medication.30
Despite the similarities, there are some characteristics that can be helpful to differentiate the two diseases. ILO stridor may sound similar to wheezing in asthmatic patients,1 but several studies performed sound analysis and concluded that in ILO, the sound originates in the neck and expands bilaterally over both lung fields.8,31,32 Auscultation is usually sufficient to determine the origin, as ILO is more prominent over the neck.1 Another differentiating factor is the abrupt onset of ILO and sudden resolution as the trigger is removed, contrasting with continuous worsening of the symptoms, when not treated, in asthma.8
Discriminating ILO from asthma is not an easy task due to the overlapping symptoms and common triggers, but determining the correct diagnosis is imperative for establishing the correct management. Kramer et al. describe a decrease of 79% of asthma medication in VCD adult patients after the correct diagnosis and treatment were established.30
Exercise-induced laryngeal obstruction
EILO is a condition where inappropriate glottic or supraglottic closure occurs during exercise, and is sometimes mistaken for exercise-induced bronchoconstriction (EIB). EILO produces inspiratory symptoms, while airway obstruction inside the thoracic cage produces expiratory symptoms. In EILO, symptoms typically peak during exercise, contrasting to EIB, where symptoms typically peak 3–15 minutes after exercise.33 EIB and EILO are not mutually exclusive, as reported by Johansson et al. in a population of adolescents with exercise-induced dyspnoea.13 Only 39.8% of the patients had EIB, 6% had exclusively EILO and 4.8% had both conditions.13 The mechanisms involved in EILO may include a combination of changes in airflow velocity, turbulence and the strength of the supporting structures; laryngeal hyper-reactivity and changes in reflex interaction; laryngopharyngeal reflux and environmental conditions. However, none of these factors have been substantiated by adequate research.33
Diagnostic criteria of inducible laryngeal obstruction
Clinical signs and symptoms
The main symptoms of ILO are dyspnoea, stridor and wheezing. Cough, chest tightness, throat tightness, and voice change between episodes are described.8,13,18,22 Episodes may be abrupt and frightening for patients and their families, leading to emergency department visits.22 When patients are evaluated during exacerbations, a high-pitched inspiratory sound will be found, but when asymptomatic, they usually have normal examination. Sometimes patients describe light-headedness, visual changes, extremity numbness and tingling during episodes associated with hyperventilation.8
In pre-verbal children ILO can manifest as intermittent stridor and respiratory distress during sleep or when awake, following emesis, crying or sphincter incontinence.23 In older children the clinical presentation can include episodic inspiratory stridor and occasionally, expiratory stridor, and children experience the primary area of tightness in the throat/larynx. In adolescents ILO commonly presents as exertional dyspnea.1,22 Symptoms cease when the trigger is removed and are likely to recur shortly after resuming the same activity.23
Rhinolaryngoscopy
The recommended procedure for diagnosing ILO is direct visualisation of paradoxical vocal cord motion, through laryngoscopy.1 In the absence of symptoms, rhinolaryngoscopy may not be diagnostic in up to 60% of the patients,27 and a provocation test is often necessary to elicit ILO symptoms.8,18,22 The choice of the test depends on the patient history and includes the use of methacholine, histamine, exercise, breathing manoeuvres and specific irritants that clinically induced symptoms.9,18 Flexible laryngoscopy is necessary to evaluate supraglottic and glottis anatomy, and demonstrate supraglottic prolapse, appearance of the laryngeal mucosa with chronic inflammation (erythema and inflammation) and movement of the glottis to include the true vocal cords, false vocal cords, arytenoids and surrounding structures.8
Christopher et al. described the classic finding for ILO as an inspiratory vocal cord adduction of the anterior two-thirds with a posterior diamond-shaped chink.5 An inspiratory closure of vocal cords greater than 50% is sufficient for diagnosis, and in some patients adduction during both inspiration and expiration can be found, as well as adduction of the false vocal folds.5 When exercise is a suspected trigger of ILO, provocation with exercise may be helpful to establish diagnosis.3,8 Laryngoscopy is usually executed promptly after exercise, but the diagnosis can still be missed if symptoms resolve rapidly.34 In this case, a continuous laryngoscopy exercise test is recommended, with laryngoscopy being performed during exercise, although it can be difficult to perform in paediatric patients.1,33
Pulmonary function testing
Spirometry is usually normal in asymptomatic patients, and some authors question its usefulness in diagnosing ILO.8,18 A provocation challenge test with the trigger may be required. The pulmonary function test (PFT) can reveal a decrease in forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC), with normal FEV1/FVC ratio.3 A common characteristic of ILO is a flattened inspiratory flow volume loop, corresponding to variable extra thoracic obstruction.8,9,18 This finding is extremely helpful to make the diagnosis in symptomatic patients, but it is not a sensitive indicator of ILO in the asymptomatic ones.3,10 ILO patients can also present an increased ratio of forced expiratory to inspiratory flow at 50% of vital capacity, as an indication of airflow obstruction during inspiration.8,18,22
Other non-invasive techniques have recently been studied for the diagnosis of EILO, such as whole-body plethysmography, mechanical modelling of the airways to determine oscillatory resistance, and videography. Larger case-controlled studies are necessary to evaluate the reliability of these techniques, specifically in patients of paediatric age.18
Differential diagnosis of inducible laryngeal obstruction
In addition to poorly controlled asthma or exercise-induced bronchoconstriction, other diagnoses have to be taken into account when ILO is considered. Anatomical defects such as laryngomalacia, frequent in childhood, when the cartilages of the posterior larynx are flaccid and fall to front and posteriorly into the airway during breathing, can cause airway obstruction and noisy breathing.23 Bilateral vocal cord paralysis is the second most common cause of stridor reported in newborns, describing the paralysis of the vocal cords in a paramedian position. The Bernoulli effect, when the vocal cords are passively sucked during inspiration, may be misunderstood as an active adductory movement.14 Recurrent respiratory papillomatosis in preschool and school-aged children can create obstruction with exercise or resting.23 Vocal cord polyps, subglottic stenosis and laryngeal oedema can occur with the same symptoms. Neurologic problems, including vagus or recurrent laryngeal nerve injury, or amyotrophic lateral sclerosis, can also share the symptoms.9,18,19,23 Differential diagnoses can also include brainstem compression and nuclear or lower motor neuron injury as movement disorder, especially in children.23 ILO is different from laryngospasm, where complete closure of the cords occurs, and happens suddenly and in an intense way.8 Other functional diagnoses must be distinguished from ILO, such as spasmodic or muscle tension dysphonia, panic attacks, Munchausen syndrome, chemical sensitivity or somatoform disorders.8
Management of inducible laryngeal obstruction
There is controversy about the management of ILO, and no consensual published guidelines. The first step after diagnosis is to reduce or stop unnecessary treatments and inform the patient of the techniques and therapeutics available to them.8,15,16 Video-recorded proof of ILO may be used as a therapeutic measure to help patients improve their understanding about the condition.15,16,33 Triggers should be identified, treated and controlled,9,15,16 and long-term treatment of comorbidities is important. If GERD symptoms are present, proton pump inhibitors should be considered.8,18
The management of this complex and multifactorial pathology needs a multidisciplinary team, which may include paediatricians, allergists, otolaryngologists, pulmonologists, gastroenterologists, paediatric psychiatry, speech and respiratory therapists, among others.9,15 A treatment algorithm was proposed by Maturo et al., recommending speech therapy as first-line treatment for patients with exercise-induced symptoms, and biofeedback treatment for the patient’s symptoms at rest, or a combination of both if first-line treatment failed to induce resolution.26
Breathing techniques that include throat relaxation and diaphragmatic breathing, and cough or throat-clearing suppression can be trained by respiratory therapists or speech and language therapists, with significant improvement in symptoms.9,16,34 Relaxation techniques should be used to control emotional and stress disorders.18 It is important to promote the comfort of children and caregivers, and explain the effectiveness of a behavioural approach to treatment, especially if they have lived with an asthma diagnosis and treatment previously. In a study of 20 adolescent female athletes, Sullivan et al. found that 95% were able to control their symptoms after 6 months of speech therapy, and 45% indicated no longer needing breathing techniques during exercise.35
Continuous positive airway pressure and heliox (70% helium and 30% oxygen) have been tried in severe symptoms,9,18,22 and in one study, showed effectiveness in 4% of patients.18 Heliox is less dense than ambient air and can maintain efficient laminar airflow during upper airway obstruction, helping to avoid intubation in severe symptoms.22 Other treatments are available for EILO, such as ipratropium bromide inhaler and inspiratory muscle training.12,16,33 Thyroarytenoid muscle botulinum toxin injections and surgical treatment can be used in selected ILO patients and in EILO,10,12 but it should be reserved for severe and refractory cases.6,10,33
The majority of children respond rapidly to the treatment plan, and those who need longer treatment should be evaluated for poor caregiver support; medically complex presentation; failure to adhere to the medical, pharmaceutical and/or behavioural plan prescribed; and inadequate or insufficient pharmaceutical treatment of comorbidities.23 With proper treatment and therapy, the long-term outcome is the resolution of symptoms. Without treatment, the symptoms persist and patients with ILO live with the inherent limitations.18
Conclusion
ILO is a complex disorder of the larynx, and a cause of dyspnoea and noisy breathing. This disease can be a traumatic experience for patients and caregivers. Most often misdiagnosed as asthma, patients could be classified as having severe and refractory asthma, with consequent corticosteroid overtreatment. The diagnosis of ILO is challenging and should be based on an association of clinical manifestations, rhinolaryngoscopy features and pulmonary respiratory tests results. Exercise, laryngopharyngeal reflux and posterior drip are the more common triggers in paediatric patients. It is essential to establish an accurate diagnosis and start an individual approach on the appropriate treatment and management of the disease. Treatment includes control of triggers, relaxation techniques, speech therapy and respiratory therapy.
The long-term functional outcome of children who have proper medical and behavioural therapy is favourable. Less school absenteeism, fewer visits to the emergency department, less stress and anxiety, and greater pleasure in physical activities, are some benefits of appropriate management.
Understanding of ILO has improved over time; however, many questions remain unanswered, especially regarding aetiology and pathophysiological mechanisms. Further research is required to establish guidelines for diagnosis and treatment.