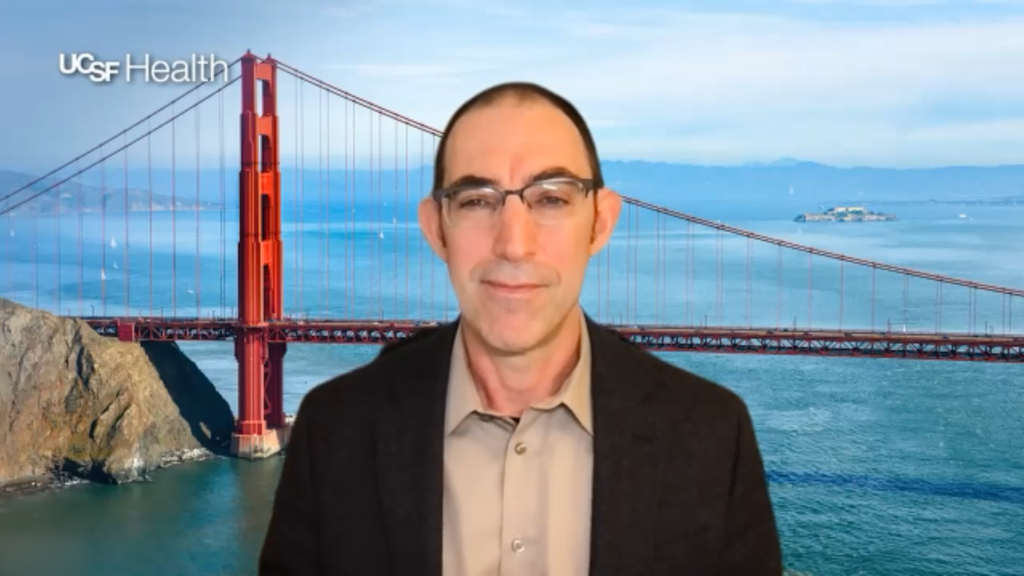
 RT234 is an investigational drug-device combination that delivers a dry powder formulation of vardenafil via a novel oscillating inhaler, designed to provide rapid, on-demand relief of breathlessness in patients with pulmonary arterial hypertension (PAH); its efficacy and clinical relevance were evaluated in a phase 2b cardiopulmonary exercise testing (CPET) trial. In this interview, Dr Raymond Benza (Icahn School of Medicine, Mount Sinai, New York, USA) discusses the limitations of current treatments for PAH, the novel mechanism of and the clinical data surrounding the RT234 drug-device combination, and future plans for a phase III trial aimed at improving patient functionality, quality of life, and survival.
RT234 is an investigational drug-device combination that delivers a dry powder formulation of vardenafil via a novel oscillating inhaler, designed to provide rapid, on-demand relief of breathlessness in patients with pulmonary arterial hypertension (PAH); its efficacy and clinical relevance were evaluated in a phase 2b cardiopulmonary exercise testing (CPET) trial. In this interview, Dr Raymond Benza (Icahn School of Medicine, Mount Sinai, New York, USA) discusses the limitations of current treatments for PAH, the novel mechanism of and the clinical data surrounding the RT234 drug-device combination, and future plans for a phase III trial aimed at improving patient functionality, quality of life, and survival.
The abstract “A Single Dose of RT234, Vardenafil Inhaled via the Axial Oscillating Sphere Dry Powder Inhaler (AOS™ DPI), Acutely Improves Exercise Capacity and Reduces Dyspnea in Pulmonary Arterial Hypertension (PAH) Patients (WHO Group 1 PH) – Results From the Open-label Phase 2b CPET (Cardiopulmonary Exercise Testing) Study (NCT04266197).” was presented at ATS 2025 International Conference, San Francisco, 16–21 May.
Q. How does PAH impact the daily lives of patients, and what are the limitations to the current treatment paradigm?
We have made great strides in improving the mortality of patients with PAH; we’ve actually tripled their life expectancy in the last decade or so and we have converted the disease from one that is very fatal to one that is very morbid. Our morbid events include hospitalizations and, most importantly to our patients, continued functional impairment. Despite our best drugs, most of our patients still reside in functional class two or three, meaning that they are breathless doing ordinary household activities or that just above household activities. So our patients remain quite impaired and this really affects their quality of life.
Q. Could you describe the mechanism of action of the drug-device combination RT234?
The interesting thing about this new therapeutic is that it really combines a novel dry powder formulation of vardenafil and a very unique oscillating inhaler. The combination of both the product itself and the inhaler allows for very deep penetration of the product to the lung. That hopefully will result in improvements in functional activity for the first time on a pro re nata (PRN) basis and that’s really the importance of the drug device combination and its application. All three things are very novel; a formulation and a meter that allows for deep penetration of the lung, and for the first time ever, a novel PRN drug for breathlessness in PAH, very similar to what asthmatics use with inhalers that they can carry in their pocket when they try to do more activity.
Q. What were the objectives and methodology of the phase 2b CPET study?
Our objectives were to try to utilize this novel, drug-device combination to improve functional capabilities of our patients as measured by cardiopulmonary exercise testing, specifically VO2 max and VE/VCO2 as a surrogate of how a patient functions, but also very importantly to measure how it improved breathlessness by looking at the Borg Dyspnea Scale conducted during 6-minute walk tests.
Q. What were the findings of the study, and what was the clinical significance of these findings?
Well, it was very interesting. First, it did reach its primary endpoint, which was an improvement in peak VO2. Now, this is very important because the way the trial was structured was looking at three different doses, 0.5mg, 1mg, and 2mg, and we saw very early that there was a definite dose response in terms of improvement in VO2, so much so that we discontinued the 0.5mg arm and really focused on the 1 and 2mg arms. When you looked at those two arms again, there was an important dose-related increase both in the mean and median VO2, reaching statistical significance in the 2mg dose. When you look at the VE/VCO2 and the Borg Dyspnea Scale, which were the secondary endpoints of the study, we saw something very similar. Again, there was a dose-related increase in the mean and median decrease in VE/VCO2 reaching statistical significance in the 2mg dose and when we looked at the Borg Dyspnea Scale, again, a very important dose-related improvement in levels of dyspnea reaching significance at the 2mg level.
The incremental increase in VO2 and decrease in VE/VCO2 is really what I would call in the avenue of clinical relevance. What I mean by that is if you look at all the patients who had the 1mg and 2mg dose and define a response as any improvement in VO2 or VCO2, again you see this nice incremental dose-related increase in the number of people defined as a responder. When you look at these responders and look at how much they increase the VO2, you could see it was on an increment of greater than or equal to 0.7mL/Kg/minute or greater than 6% from baseline. Both these two changes when you look at the literature are considered clinically significant. A 6% increase in VO2 max is usually associated with a drop in mortality and an increase of at least 0.7mL/Kg/minute is associated with the equivalent of a minimal meaningful increase in 6-minute walk distance of around 30 meters.
So, translating the results into changes we saw, it seems that this will be clinically relevant to our patients and how they function. One of the interesting things that we did as a correlator to this is we did a very thorough job looking at the incremental changes in VO2 max that requires a patient to move from one daily activity to something requiring slightly more breathfulness, for example, walking outside to carrying garbage outside. When you look at those incremental increases in activity and what they require in terms of increasing VO2, it’s on the order for around 0.7mL/Kg/minute. If you can extrapolate that to what this will transpire for our patients, it should be that after an inhalation, they’re able to do the next level of activity that they weren’t able to do at baseline.
Q. What are the next steps in the development of RT234?
Well, I think what we want to do is construct a very meaningful phase III trial that really hits all the top 3 correlates for our regulatory authorities and for our patients, and that means trying to design an endpoint that shows that our new product will improve the way a person functions, feels, and survives. Looking at similar changes in activity levels measured in conjunction with a patient-reported outcome, something that really tells us how the patient’s quality is changed with the product, and looking at drops in risk scores like the REVEAL risk score, which is a surrogate for survival, are some of the things that we’re looking at for our phase III trial.
Transcript has been autogenerated.
Further content in pulmonary hypertension.
Editor: Victoria Jones, Senior Content Editor.
Cite: Raymond Benza. Findings from a Phase 2b Trial Evaluating RT234, a Drug-Device Combination for Pulmonary Arterial Hypertension: Raymond Benza, ATS 2025. touchRESPIRATORY. 25 June 2025.
Abstract: Benza RL, Staehr P, Franco V, et al. A Single Dose of RT234, Vardenafil Inhaled via the Axial Oscillating Sphere Dry Powder Inhaler (AOS™ DPI), Acutely Improves Exercise Capacity and Reduces Dyspnea in Pulmonary Arterial Hypertension (PAH) Patients (WHO Group 1 PH) – Results From the Open-label Phase 2b CPET (Cardiopulmonary Exercise Testing) Study (NCT04266197). Am J Respir Crit Care Med. 2025;211:A7048.
Disclosures: This short article was prepared by touchRESPIRATORY in collaboration with Raymond Benza. touchRESPIRATORY utilize AI as an editorial tool (ChatGPT (GPT-4o) [Large language model]. https://chat.openai.com/chat.) The content was developed and edited by human editors. No fees or funding were associated with its publication.
Raymond Benza discloses consulting for United Therapeutics, Gossamer, Insmed, Abbott, Tectonic, Bayer; and receiving grant/research support from United Therapeutics, Gossamer, Insmed, Abbott, Tectonic, and Bayer.
Register now to receive the touchRESPIRATORY newsletter!
Don’t miss out on hearing about our latest peer reviewed articles, expert opinions, conference news, podcasts and more.