Acute respiratory tract infections (RTIs) affect children and adults with chronic respiratory conditions throughout the world, and are associated with significant morbidity and mortality.1 Acute RTIs are one of the leading causes of mortality in both children and adults, with an estimated 3.5–4 million deaths per year attributed to both acute upper and lower RTIs.2,3 Recurrent RTIs are especially common in young children, affecting up to 25% of children <1 year of age and 18% of children 1–4 years of age.1 Paediatric RTIs also incur substantial healthcare costs; they frequently cause complications that necessitate multiple medical visits, accounting for nearly half of all paediatric consultations in developed countries, and are among the leading causes of paediatric hospital admissions in the US.1 Furthermore, although many RTIs have viral aetiology, they are still a leading cause of antibiotic prescriptions, thereby contributing to the development of antibiotic resistance and further increasing healthcare costs.1,4 Overall, despite the availability of healthcare in developed countries, RTIs still exert a substantial clinical and economic burden and represent a clear unmet medical need.1
Prevention of RTIs can be difficult, as the risk factors are many and varied, including sociodemographic (partial immunisation, overcrowding), nutritional (malnutrition) and environmental aspects, as well as clinical risk factors, such as minor immunodeficiencies.5–7 However, the use of immunostimulants or immunomodulator therapies may provide an alternative therapeutic option that is complementary to vaccination.8
Bacterial lysates, such as OM-85, are produced by chemical or mechanical lysis of specific bacterial cultures. As such, they contain conserved pathogen-associated molecular patterns (PAMPs) for these bacteria, which have the potential to activate the cellular constituents of innate and adaptive non-specific loco-regional immune responses.9–12 This can lead to the induction of not only specific, but also non-specific loco-regional immune responses, with polyclonal production of immunoglobulins.10–13 Therefore, lysates of bacteria from the respiratory tract may provide clinical benefit in patients with recurrent RTIs, regardless of the viral or bacterial aetiology, in different patient populations with infectious exacerbations of inflammatory respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD).
Here we discuss the concept of a bacterial lysates class effect and review the clinical relevance of the bacterial lysates OM-85, with a focus on its efficacy and safety profile in various paediatric and adult populations.
Bacterial lysates – is the class effect concept applicable?
Pharmacological compounds are often grouped into ‘classes’, where each drug has similar properties or structures, and can be broadly categorised into five types based on the shared aspects: chemical, mechanistic, biomarker, outcome and genotype. The extrapolation of knowledge from one class member to another has become increasingly common; a concept known as a ‘class effect’. An early example of a class effect was provided by Vaughn Williams et al., who grouped various anti-arrhythmic medications into separate classes based on their electrophysiological characteristics.14 However, while it is of practical merit to conceptualise a class effect, experience has shown that class may not always predict outcomes (e.g. there was no relationship between the Vaughan Williams anti-arrhythmic classifications and patient outcomes),14 and clinical outcomes may differ greatly for agents within a class. For example, non-steroidal anti-inflammatory drugs have been shown to have markedly different inhibitory ratios of cyclooxygenase 1 and 2, yet a similar risk of myocardial infarction,15 and the endothelin receptor antagonists ambrisentan, bosentan, sitaxsentan and macitentan exhibit significantly different levels of hepatotoxicity (as measured by hepatic transporter inhibition and accumulation in hepatocytes).16 With regard to bacterial lysates, the concept of a class may not be applicable due to considerable variations in their composition, manufacturing process and activity/mode of action (see Table 1).10

Therefore, for bacterial lysates, class may not automatically translate into a class effect, and therapeutic decisions for these compounds should always be based on clinical evidence (i.e., efficacy and safety data). An overview of the level of clinical evidence available for key bacterial lysates is provided in Table 2.

OM-85 is the product of alkaline lysis of 21 strains of eight species of common bacterial respiratory tract pathogens: Haemophilus influenzae, Streptococcus pneumoniae, Klebsiella pneumoniae, Klebsiella ozoneae, Staphylococcus aureus, Streptococcus pyogenes, Streptococcus viridans and Moraxella catarrhalis.10 The active ingredients of OM-85 retain their activity following gastric transit, as well as their cell activation capacity following gastric-buffer incubation.13 The resultant non-specific potentiation of the immune system may help to protect against both viral and bacterial respiratory infections and, as discussed in more detail later, may also provide additional clinical benefits in inflammatory conditions such as asthma and COPD by balancing immune responses via downregulation of Th2-mediated airway hyperreactivity/inflammation and stimulating the release of anti-inflammatory cytokines.10,11
OM-85 – mechanism of action
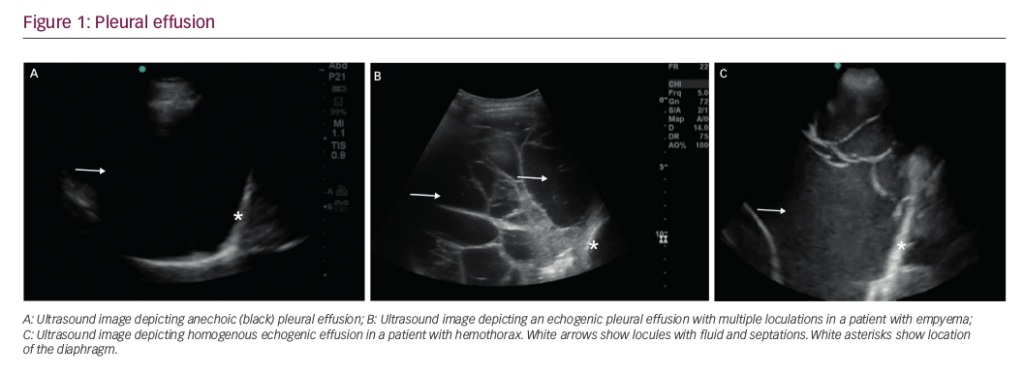
The rationale for the use of orally administered immunomodulators for the prevention of RTIs is focused around the sampling of specific antigens by microfold (M) cells and dendritic cells in gut-associated lymphoid tissue (GALT).10 In the case of OM-85, antigen sampling by M cells in GALT Peyer’s patches in the small intestine initiates mucosal immunity responses, allowing for transport of microbial antigens across the epithelial cell layer from the gut lumen to the lamina propria where interactions with dendritic cells can take place (Figure 1A).10–12 This leads to maturation of mucosal dendritic cells into antigen presenting cells, which initiate immune cascades that involves the downstream activation of cellular constituents of both the innate and adaptive branches of the immune system.10,12 These downstream events include:
- the activation of monocytes and natural killer cells;
- the activation of T cells (T-helper [Th] 1 cells, T-regulatory [Treg] cells and cytotoxic CD8+ cells);
- the expression of anti-microbial peptides in epithelium and mucosa;
- the activation of macrophages;
- the migration of polymorphic neutrophils to the lung;
- the expression of B-cell and antiviral Th1-related cytokines (via selective induction of nuclear factor [NF]);
- B-cell maturation (leading to an increase in serum and airway immunoglobulins); and
- the promotion of immune system maturation in children via downregulation of Th2 and restoration of Th1/Th2 imbalance through activation of Treg cells (Figure 1B).10–12

This, in turn, may result in the homing of immune cells to bronchial-associated lymphoid tissue in the lungs and subsequent polyclonal antibody production, facilitating immune responses against viral and bacterial RTIs.10,11 In addition, OM-85 has been shown to have broader immunomodulatory effects. These include:
- an antiviral effect via the induction of interferon-α and interferon-β and a dual effect on interleukin (IL)-1 production (downregulating IL-1β during an inflammatory state, thereby controlling inflammation, but inducing pro-IL1β in the absence of a strong inflammatory state), indicating that OM-85 favours a protective primed immunological state while dampening inflammasome activation in specific conditions;17,18
- the stimulation of cytokines, such as IL-6 and tumour necrosis factor-alpha (TNF-α), indicating an enhanced clearance ability of macrophages against invading bacteria;19
- increasing the levels of CD4+, CD25+, Foxp3+ and Tregs in airway mucosal tissues, attenuating airway inflammation and hyperresponsiveness;20 and
- the selective induction of NF-κβ and MAPK in dendritic cells, thereby upregulating chemokines involved in the migration of macrophages and neutrophils, as well as upregulating B-cell activating cytokines such as IL-10, which may control excessive expression of pro-inflammatory mediators and tissue damage in patients with COPD.18
In summary, the effects of OM-85 have been well characterised and its mode of action is sophisticated and multifactorial, distinct from the antigen-specific action of vaccines (i.e., the production of specific antibodies by B cells).10,21
OM-85 – safety profile
OM-85 has a favourable safety profile that is supported by nearly 40 years of clinical experience and pharmacovigilance monitoring.22 Cumulative pharmacovigilance data from 1979 up to 31 October 2017 show that from an estimated OM-85 exposure of ~100 million patients, only 1,974 adverse event reports (unsolicited and solicited) have been received and registered in the safety database (OM Pharma; data on file). From this safety database, important identified risks were shown to be limited to hypersensitivity reactions (Standardised MedDRA Query23), with 538 cases reported. The majority of these hypersensitivity reactions were classified as non-serious (~85%) and were localised to the skin (e.g. pruritis, rash, urticaria, erythema, hypersensitivity; these accounted for 57% of all reports). In total, 28 severe adverse cutaneous reaction reports were registered in the safety database (OM Pharma; data on file), with only three instances of toxic epidermal necrolysis or Stevens-Johnson Syndrome reported in patients receiving OM-85 in nearly 40 years. Further, no relationship with OM-85 administration and these events was established, and therefore no safety signal was validated.
These data support the findings from placebo-controlled clinical trials, where OM-85 has demonstrated a favourable safety profile (similar to that of placebo in most studies) in the prevention of RTIs in children,24,25 the management of atopic dermatitis in children,26 and the prevention of exacerbations in adults and the elderly with chronic lung inflammatory disease such as chronic bronchitis and/or COPD.27,28 Indeed, a meta-analysis of data from eight clinical trials investigating OM-85 for the secondary prevention of recurrent RTIs reported similar rates to placebo for minor adverse events (17.7% versus 18.2%; OM-85 versus placebo, respectively), serious adverse events (1.0% versus 0.5%), and study withdrawals due to adverse events (1.3% versus 0.7%).29 No causal relationship was established for any of these adverse events, no laboratory abnormalities were reported and no deaths attributed to study medication.29
Controversies – potential interference with vaccines
There are two main concerns that have been raised regarding bacterial lysates and vaccinations: that bacterial lysates, such as OM-85, might contribute to a reduction in vaccination coverage rates, as they contain bacterial antigens such as S. pneumoniae and H. influenzae and could therefore be incorrectly regarded as a substitute for vaccines against these pathogens; and that the administration of bacterial lysates alongside vaccines may impact the immunogenicity and/or tolerability of the vaccine itself.
With regard to the potential reduction in vaccination rates, there is no robust evidence of immunostimulants or immunomodulators being prescribed as an alternative to active immunisation in Italy or other countries. Indeed, bacterial lysates are typically used to reduce the risk of respiratory infection as a complementary strategy to other preventative measures such as vaccination.30 As such, the authors feel that a reduction in vaccination coverage rates due to OM-85 use would be unlikely.
With regard to the impact on the immunogenicity and/or tolerability of vaccines, the mechanism of action of OM-85 is distinct to the antigen-specific effect of vaccines (non-specific potentiation of the immune system versus production of specific antibodies by memory B cells, respectively),10 indicating that any interference is unlikely. This hypothesis is supported by the results of a prospective, randomised, single-blind study conducted by Esposito et al. of children affected by recurrent RTIs.31 In total, 68 children 36–59 months of age were vaccinated with an inactivated influenza vaccine either with (n=33) or without (n=35) concomitant OM-85 (administered using a standard 3 x 10 dosing regimen [see clinical evidence section for further details]).31 Overall, the inactivated influenza vaccine was shown to be effective in stimulating an immune response to help prevent infection in children.31 Co-administration of the vaccine with OM-85 was found to have no significant effect on influenza vaccine-induced seroconversion or seroprotection rates, geometric mean titres, the number of dendritic cells or the presence of plasmacytoid dendritic cells.31 In addition, OM-85 did not significantly change the pool of memory B cells that produce immunoglobulin G and immunoglobulin M antibodies against influenza antigens, both of which were significantly increased post-vaccination (~3–4 fold increase, p<0.01 for both immunoglobin isotypes).31 However, compared with the administration of vaccine alone, respiratory morbidity and antibiotic use was significantly reduced in patients receiving both vaccine and OM-85 compared with patients receiving only vaccine, suggesting an added therapeutic benefit when combining the two complementary preventive measures (Figure 2).31 The incidence of adverse events was nearly similar between the OM-85 and no OM-85 treatment groups (15.2% versus 20.0%, respectively), both for local reactions (12.1% versus 17.1%) and systemic reactions (6.0% versus 11.4%), with no serious adverse events reported.31 This demonstrates the favourable tolerability profile of OM-85 in combination with an inactivated influenza vaccine. Similar results have been reported in a study of 396 elderly patients (≥65 years of age) receiving influenza vaccination with OM-85 (n=147) or without OM-85 (n=143).28 No significant difference between groups was observed in circulating immunoglobulin concentration or intercurrent medical events, with no specific side-effects reported.28 In addition, a 28% reduction in both lower RTIs and antibiotic use was reported with OM-85 (compared with influenza vaccination alone).28 Supporting the clinical study findings, no safety issues have been reported relating to the concomitant administration of OM-85 and influenza vaccines in post-marketing pharmacovigilance surveillance (OM Pharma; data on file; cumulative pharmacovigilance safety database from 1979 to 31 October 2017). Further, based on present general knowledge, preclinical and clinical studies, and post-marketing surveillance, there does not appear to be any evidence of interaction between OM-85 and any vaccines, of either bacterial (e.g. Haemophilus influenzae, Streptococcus pneumoniae) or viral (e.g. trivalent or tetravalent live attenuated vaccines, such as measles, mumps, rubella and/or varicella [MMR/MMRV]) origin.

In conclusion, it is the authors’ opinion that vaccination schedules for children over 12 months should not be altered when administering the bacterial lysates OM-85, as restrictions on the concomitant use of OM-85 and vaccines (or intervals in the administration of either) are not supported by clinical evidence.
Controversies – potential risks in atopic or asthmatic patients
As described earlier, there is an established mechanistic and clinical rationale for the use of non-specific immunomodulators as prophylaxis against RTIs.10,11 In addition, the immunoregulatory properties of OM-85 support its use in patients with an atopic condition such as poorly controlled asthma; the OM-85-induced modulation of Treg cells could potentially lead to more efficient viral clearance and a downregulation of inappropriate Th2-associated immune responses, which are central to the airway hyper-responsiveness and inflammation during asthma exacerbations.10,12 In line with this hypothesis, a number of studies have shown that prophylaxis with OM-85 in paediatric patients with a history of recurrent wheezing or asthma can significantly reduce the incidence of exacerbations triggered by infections and wheezing episodes (by ~30–50%; p<0.05),32–34 RTIs (by ~30–40%; p<0.01),32,33 and antibiotic use (44% [days]; p<0.01).32 In addition, OM-85 was shown to have a favourable safety profile in the studies that reported safety data, with adverse events occurring at a similar incidence to placebo/control groups (~5–10%) and no severe events or events leading to treatment discontinuation reported.32,33
Clinical evidence and relevance of OM-85 in the prevention of respiratory tract infections
Respiratory tract infections in the paediatric population
Clinical study data have shown OM-85 to be effective for the prevention of RTIs in children for at least 6 months (up to ~35–40% reduction) irrespective of aetiology.24,25,32–36 Additional clinical benefits have also been reported for recurrent otitis media and acute bacterial tonsillitis.24,35,37 Dosing regimens vary between these studies, but the most commonly used regimen involves administering one capsule (containing 3.5 mg of lyophilised bacterial lysates) every morning for the first 10 days of each month for 3 months.29 A second round of 3 x 10 doses can also be administered 6 months after the first dose.24,29 A meta-analysis, as well as other combined study analyses, supports the results of these individual clinical trials, showing that OM-85 can significantly and consistently reduce the incidence of recurrent paediatric RTIs by 36% and that OM-85 provides the greatest benefit in preschool children and patients with a history of very frequent RTIs.29,36,38,39 In addition, by preventing RTIs and/or bacterial complications, OM-85 has also been shown to reduce antibiotic use and provide cost-savings for the community and healthcare services.40
Despite the burden exerted by recurrent RTIs, there are no formal international guidelines for the treatment and management of recurrent RTIs per se. In children, there are currently only guidelines for the treatment of specific paediatric conditions (such as otitis media), and while most of these recommend avoiding antibiotic overuse in the treatment of paediatric RTIs by adopting preventive measures, they do not specify what these measures might be. Clinical evidence indicates that OM-85 could address both of these issues, by reducing the frequency of RTIs and antibiotic use.1,29,36,38,40 Indeed, a number of expert consensus/position/opinion papers now discuss and/or recommend the use of bacterial lysates and OM-85 as effective measures for preventing RTIs in children.1,41,42
Based on available clinical data and meta-analyses, the authors propose three key recommendations for the use of OM-85 in the prevention of recurrent RTIs in paediatric patients:
- that OM-85 is considered in children 2–6 years of age who are at the highest risk of RTIs, as OM-85 appears to confer the greatest benefit in these patients (Figure 3);
- that OM-85 is considered for the prevention of viral RTIs, as its clinical efficacy is not limited to the prevention of bacterial RTIs; and
- that the use of OM-85 is not limited by the concurrent administration of vaccines.

Adult population
COPD is a major public health challenge and a leading cause of chronic mortality and morbidity, which is predicted to become the third largest global cause of death by 2020.43 The main goals for the treatment of COPD are to reduce symptoms and prevent future exacerbations (acute episodes of disease worsening), which are associated with a worse prognosis, reduced quality of life and increased mortality risk.43 Because of the increased morbidity and mortality risk, patients with COPD who experience frequent exacerbations require additional treatment beyond symptomatic control.
As the large majority (~50–80%) of COPD exacerbations are associated with bacterial or viral respiratory infections,44 targeting specific molecular pathways to prevent viral/bacterial infection and reduce inflammation could therefore help prevent or mitigate COPD exacerbations. As such, OM-85 provides a complementary and effective therapeutic option for adults with COPD who experience frequent exacerbations (via modulation of the lung immune response), potentially reducing hospitalisations and the use of antibiotics.45 Data from clinical trials support this hypothesis, with several studies reporting significant reductions in exacerbations, decreased severity of exacerbations and reduced antibiotic use/hospitalisation in patients with COPD or chronic bronchitis receiving OM-85 treatment.27,28,46–49 In addition, a meta-analysis by Pan et al. reported OM-85 to be associated with a 20% reduction in COPD exacerbations and a 39% reduction in antibiotic use.50 However, no significant effect was observed on the severity of exacerbations or duration of hospitalisations.50 Nevertheless, as healthcare costs and resource utilisation associated with COPD and other chronic respiratory conditions are high, incorporating OM-85 into an integrated care programme has the potential to reduce these costs and optimise disease management and patient outcomes.51,52 Indeed, OM-85 is included and recommended (Grade A) in treatment guidelines for acute and chronic rhinosinusitis in adults without nasal polyps, and could also provide benefits in these patients.53,54 In addition, the use of bacterial lysates is mentioned in the current Global Initiative for Chronic Obstructive Lung Disease (GOLD) document with respect to the potential benefits of reducing exacerbations in COPD.43
Overall, considering the available clinical data and meta-analyses, the key recommendations and conclusions based on author consensus are:
- that OM-85 be used in patients with COPD, as it has been associated with a reduction in exacerbations triggered by infection, and antibiotic use;
- that of these patients, OM-85 may show the greatest treatment response in those with a high frequency of exacerbations (i.e., those with the greatest risk of morbidity and mortality); and
- that OM-85 could provide a cost-effective means of reducing COPD exacerbations.
Clinical relevance of OM-85 within the context of increasing antibiotic resistance
Antibiotic resistance is an increasing problem, with new strains of resistant bacteria continuing to emerge and ~25,000 deaths attributed to specific antibiotic resistant bacteria in the EU in 2007.55,56 With few alternative antibiotic options available and/or in development, there are only two viable approaches to overcome this problem: improving the use of current antibiotics and reducing the number of infections. Unfortunately, the overuse and misuse of antibiotics in paediatric patients is still a common issue despite attempts to increase awareness and education.4,57 As such, reducing the number of infections (and in turn antibiotic use) may be the most viable option. Furthermore, antibiotic treatment is an important perturbing factor of the microbial equilibrium of both the gut and respiratory microbiota throughout life.58 In children this has been shown to decrease the abundance of presumed beneficial commensal bacteria in the upper respiratory tract, which might increase the risk of RTIs following antibiotic treatment.58 OM-85 may help address these issues, as it represents a way to reduce antibiotic use, especially in patients with a higher risk of RTIs requiring antibiotics, such as those with COPD.28,32,40,48,50
Overall, the authors recommend implementation of antibiotic stewardship that includes prophylaxis with immunomodulatory agents of choice, as this may help to reduce both the appearance of antibiotic resistance and perturbations of gut and respiratory microbiota.58,59
Immunomodulatory properties of OM-85 – current understanding and future perspectives
Because immunological responses are highly complex, the targeting of multiple molecules/pathways (rather than a single molecule/pathway) is usually required in order to achieve a beneficial immunomodulatory effect. OM-85 targets multiple pathways and has a broad range of immunological effects, including Treg cell expansion in the airways.10,60 As such, it is hypothesised that OM-85 may promote a re-organisation of gut and lung microbial communities, improving cross-talks with immune effectors that favour immune homeostasis and reducing disease exacerbations and antibiotic use.58 However, while our understanding of microbial ecology has increased dramatically over recent years, much remains to be understood about how different microbial groups influence various arms of host immune defence, and further studies are required to characterise the effect of OM-85 treatment on these interactions.58,61
Discussion
While OM-85 is classified as part of the bacterial lysates family, it has been shown to possess its own distinct and multifactorial mode of action, causing maturation and activation of gut mucosal dendritic cells, homing of immune cells to lymphoid tissue in the lungs and activation of cellular constituents of innate and adaptive mucosal immune responses.10
Clinical study and pharmacovigilance data have shown that OM-85 is well tolerated in both adult and paediatric populations and that it can be used in combination with vaccines with a manageable risk profile. Clinical studies have shown that OM-85 provides clinical benefits in various respiratory conditions such as asthma, chronic bronchitis, COPD and chronic rhinosinusitis, as well as clinical efficacy in preventing both viral and bacterial RTIs and reducing antibiotic use. Based on the evidence to date, the authors believe that OM-85 can provide the most benefit to paediatric patients by
- considering OM-85 use in children 2–6 years of age who are at the highest risk of RTIs;
- considering OM-85 for the prevention of viral RTIs as well as bacterial RTIs; and
- not limiting the use of OM-85 during administration of vaccines. Preclinical evidence clarifying the mechanism of action of OM-85,10–12 together with recent clinical evidence,24,25,32–35 indicate that its use could also be extended to the prevention of recurrent paediatric infection-induced wheezing or asthma attacks, as well as providing benefits for patients with non-atopic conditions such as chronic rhinosinusitis and COPD (in adults).27,28,46–50,53,54
Overall, OM-85 represents a valuable addition to the therapeutic landscape for these conditions and may be an effective tool not only for specialists (paediatricians, pulmonologists, ear, nose and throat), but also for general practitioners.
Conclusions
In conclusion, there is growing mechanistic and clinical evidence supporting both the ability of OM-85 to promote immune homeostasis and the benefits of OM-85 therapy in various respiratory conditions such as asthma, COPD, chronic rhinosinusitis and in the prevention of RTIs. Additional research is required to further characterise the properties of OM-85 and investigate the therapeutic benefit in specific patient populations or respiratory conditions.