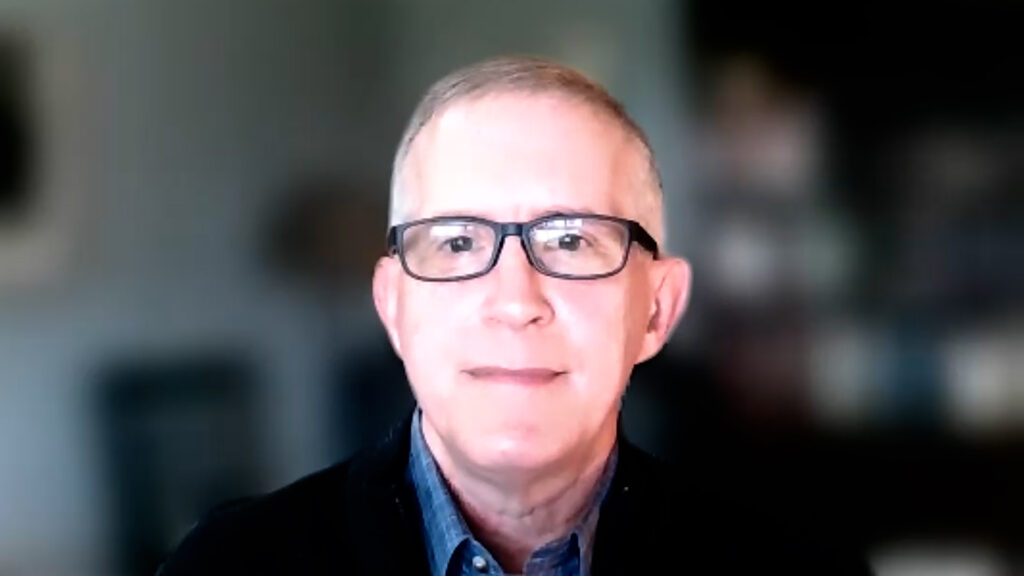
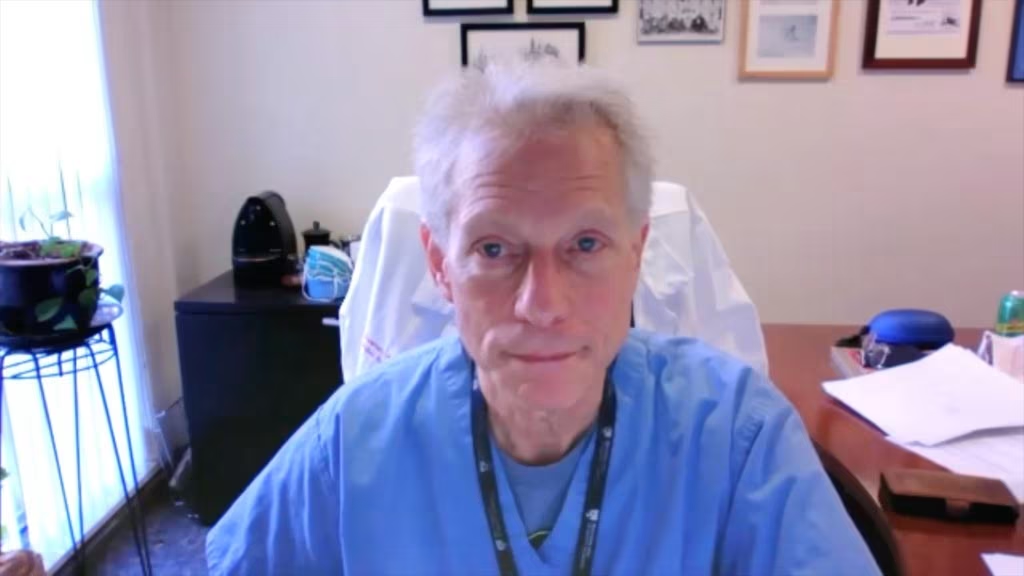
Idiopathic pulmonary fibrosis (IPF) is a serious chronic lung disease which results in symptoms such as shortness of breath and dry cough and is caused by fibrosis of the lungs. It was a pleasure to talk with Dr. Steven D. Nathan (Inova Fairfax Hospital, Falls Church, VA, USA) to discuss the incidence, prognosis and pathology of IPF, the current standard of care and the difficulties in recruiting participants in IPF clinical trials.
The abstract ‘Preliminary Baseline Data From the Teton Phase 3 Clinical Trials of Inhaled Treprostinil in the Treatment of Idiopathic Pulmonary Fibrosis. ‘ (Abstract number: P766) was presented at ATS 2023, 19-24 May 2023.
Questions
- What is the incidence, prognosis and pathology of idiopathic pulmonary fibrosis (IPF)? (0:18)
- What is the current standard of care for IPF and what are the unmet needs? (1:54)
- What difficulties are associated with recruiting participants in IPF clinical trials? (3:24)
Disclosures: Steven Nathan discloses consulting for United Therapeutics, Boerhinger-Ingelehim, Bellerophon, Gossamer, Merck, Fibrogen, and Pliant; receiving grant/research support from Tvardi; serving on advisory boards for Fibrogen, Boerhinger-Ingeheim, and United Therapeutics; and participating on speaker’s bureaus with United Therapeutics and Boerhinger-Ingelheim.
Support: Interview and filming supported by Touch Medical Media Ltd. Interview conducted by Victoria Jones.
Filmed in coverage of the ATS Annual Meeting.
Click here for more content on ILD & IPF.
Transcript
What is the incidence, prognosis and pathology of idiopathic pulmonary fibrosis (IPF)? (00:18)
The incidence of idiopathic pulmonary fibrosis, I think, is growing over time. It’s estimated in the US that there are about a hundred and fifty thousand to maybe a hundred and seventy-five thousand patients with idiopathic pulmonary fibrosis. My personal bias is that it’s actually more than this, and it might be because we work in an ILD center, so we get sent and see a lot of these patients. I probably follow around two hundred to two hundred and fifty patients with idiopathic pulmonary fibrosis. The prognosis is generally not very good. If one harkens back to the pre-antifibrotic era, which in the US was prior to 2014, in Europe and the UK, 2012 was when the first antifibrotics got approved. Prior to this, the prognosis included a median survival of anywhere from about three and a half to five years. What we’re finding now from more recent registries with the advent of antifibrotic therapy is that the median survival has increased and sits around maybe six to even eight years in terms of median survival. In terms of the pathology, it’s rather complex. We think that the fibroblast is the main driving force behind the progression of fibrosis and the therapies that we have today largely look at how to interfere with pathways affecting fibroblastic proliferation. But that’s our current thirty thousand foot view of the pathogenesis of idiopathic pulmonary fibrosis.
What is the current standard of care for IPF and what are the unmet needs? (01:55)
The current standard of care of IPF patients from a therapeutic standpoint include one of the two available antifibrotics, pirfenidone and nintedanib and these medications are variably available throughout the world. In the US, we have both of these drugs available and approved since 2014. Standard of care also includes things like supplemental oxygen when needed, pulmonary rehabilitation, looking for and addressing comorbidities should they exist, and then also referral for lung transplantation in appropriate candidates. I believe that standard of care should also be consideration of enrolment in clinical trials because clearly there’s still a large unmet need for this disease. Both nintedanib and pirfenidone have modulated the natural history of the disease, as we’ve seen with increasing survival. But clearly, there’s more room to go in terms of furthering survival benefit in these patients. Both of these drugs are approved based on preservation of lung function, but what we’re seeing from multiple registries is that these patients are living longer, but we haven’t cured the disease. So there’s certainly an ongoing unmet need for patients with idiopathic pulmonary fibrosis and hence the need to populate more clinical studies to see what the next steps forward are going to be.
What difficulties are associated with recruiting participants in IPF clinical trials? (03:24)
Even though there are IPF clinical trials around, there are some difficulties recruiting patients into these. Invariably, these studies have inclusion and exclusionary criteria. So if patients have significant comorbidities, they’re excluded. We actually looked at this and had a publication that of all of our IPF patients that we scrutinize for clinical trials, only about twenty, twenty-five percent of them qualify for clinical trials. What we’re seeing now is that there are many more clinical trials available for patients with IPF. So the trials are actually competitive with one another. So they’re competing for a finite population and if you go to any IPF clinical center that does research, we have to look at the studies we’re doing because we can’t commit to too many of them. Otherwise, you’ll be cannibalizing all the studies by having too many and being unable to recruit adequately into any of them. So the competitive landscape, I think, impedes recruitment into clinical trials. But having a competitive landscape, I think, overall, is very good for patients. The criteria to get patients into the clinical trials have loosened up somewhat compared to, say, ten years ago, where the criteria were much more stringent in terms of enrolment. So ongoing need and hopefully, I feel like enrolments in clinical trials is a way for patients to fight back against the disease as well as getting access to potential therapies before they become available in the clinical arena.
Subtitles and transcript are autogenerated