Asthma affects nearly 300 million people worldwide.1 Despite a notable decline in age-standardized prevalence, mortality and disability-adjusted life years over the past three decades, the burden of asthma remains high in many countries including low-middle-income countries.2 Climate change is also predicted to significantly impact asthma and other respiratory-related conditions, as rising global temperatures lead to longer pollen seasons and promote ground-level ozone pollution. With the increasing burden of asthma, effective management strategies will become increasingly vital to improving asthma care.3
Conventional asthma management heavily relies on the regular and correct administration of inhaled medications, particularly inhaled corticosteroids, which are essential for controlling inflammation and preventing asthma exacerbations.4 Despite the importance of adherence to inhaled medication, many patients struggle to achieve the level of adherence required for disease control or adequate inhaler technique, leading to suboptimal asthma control and poor patient outcomes.5 The Global Initiative for Asthma describes the multifactorial issue of poor adherence as ‘the failure of treatment to be taken as agreed upon by the patient and the healthcare provider’. This also encompasses proper inhaler technique, as even if patients take their medication consistently and at the recommended dose, they may not achieve ‘true’ adherence if their inhaler is not being used correctly – which is a case of inhaler competence.6 Non-adherence affects a significant portion of patients with asthma, with adherence estimates ranging from 22 to 78%.7 In addition, a 2018 systematic review found that proficiency in teaching correct inhaler technique by healthcare professionals (HCPs) was only around 15.5%, indicating an important practice gap for health professionals with patients being unable to receive adequate guidance for inhaler technique when required.8 Improper medication usage and non-adherence are often underreported or unnoticed by HCPs, making it difficult to identify patients who are struggling with these issues.9 More sensitive or objective measures, such as weighing inhaler canisters or using electronic dose counters, have limitations, including a lack of detailed adherence data and overestimations of adherence influenced by a phenomenon called ‘dose dumping’. This phenomenon refers to an attempt by a patient to disguise non-adherence, where individuals may release multiple doses of medication shortly before a study or clinic visit.9–11 Prescription records are one method that provides more accessible, retrospective data with reduced observational bias. However, they cannot identify the frequency and timing of medication use, nor can they reveal patients who collect their medication but never use their inhalers or have problems with inhaler technique.9 The accuracy of current adherence measures varies widely, and the adherence commonly reported in the literature – usually from self-report, prescribing or dispensing records – is only a proxy measure of adherence, capturing only a small extent of ‘true’ adherence (i.e. actual medication actuation and inhalation). To improve clinical outcomes and differentiate poor adherence from lack of treatment response, more specific data are required.
These statistics highlight an important gap in the effective management and support of asthma, underscoring current limitations in asthma care that may require innovative solutions to address. Possible solutions that have been trialled include personalized education and behavioural interventions, such as motivational text messages, to improve adherence.12 There have also been more niche methods trialled, such as school-based management to help increase adherence in child populations.13 While these strategies have achieved some success within a clinical trial setting, few have been implemented long-term in practice. Interventions that are multifaceted and require significant resourcing to sustain may limit transferability to the clinical setting. Digital technologies have the advantage of allowing automation and scalability, offering unique opportunities to improve asthma care not seen with
non-technological methods.14
This article explores the potential impact of smart inhalers on asthma self-management, specifically examining how these devices may contribute to improved asthma control through enhanced monitoring, adherence and optimized inhaler technique. Asthma is a prevalent chronic respiratory condition, and proper use of inhaled treatment plays a key role in effective management. Despite this, suboptimal control remains common, often due to poor adherence and incorrect inhaler technique. This article provides an overview of smart inhalers and discusses these as a promising solution to address some of the current challenges of asthma management while exploring the key opportunities, challenges and clinical implementation strategies of these devices.
The smart inhaler
Smart inhalers are one promising approach that can be used to improve adherence monitoring and personalize asthma care. While there appears to be no universally accepted definition of ‘smart inhalers’, these devices are generally described in the literature as ‘inhaler-based electronic monitoring systems that record medication usage, with or without assessing the technique of device use’.15 In addition to medication monitoring, smart inhalers offer a wide array of functionalities designed to enhance medication adherence and improve patient outcomes.16,17 Sensors can measure the frequency and timing of inhaler actuations, providing valuable data on patient usage patterns. Smart inhalers can also send reminders to patients to take their medication, supporting adherence and ensuring consistent use. Depending on the device type, adherence-promoting functions may include personalized text messages, application (app) notifications or auditory alerts from the inhaler itself.18,19 More advanced devices can also identify and monitor suboptimal inhalation techniques using information collected on flow rates, air pressure, vibration and sound wave parameters.16 With real-time feedback on inhaler use, patients can be guided towards better technique, ensuring maximal therapeutic effect from their inhaler use.
Other advanced inhaler models can correlate inhaler use with environmental and individual factors. Environmental factors may include air quality, temperature, pollen and other personal or lifestyle factors such as physical activity, which can help the patient to gain greater insight into factors contributing to their asthma symptoms and exacerbations.18,19 These data can also be linked with larger digital platforms, such as mobile apps, to facilitate personalized self-management plans. With the patient’s permission, the same data can be integrated into formalized and standardized electronic health records (EHRs). Healthcare providers can use this information to assess patients’ adherence and take these metrics as guides for effective clinically informed decisions about treatment plans.16,20
To identify opportunities and challenges for smart inhalers, we searched Cochrane Library, PubMed, Clinical Key, Embase, Web of Science and Google Scholar using key search terms such as ‘digital inhaler’, ‘smart inhaler’, ‘digital inhaler technology’, ‘medication adherence’ and ‘asthma management’. This search was performed during the months of May to July 2024, and the strategy was refined to include studies published primarily between 2000 and 2024, restricted to those in English.
Studies that focused on the use of smart inhalers in asthma management were included. Relevant outcomes included, but were not limited to, inhaler technique, adherence, patient or healthcare provider perspectives and healthcare utilization and/or implementation. Included study designs were randomized controlled trials, observational studies, systematic reviews and meta-analyses. Studies were excluded if they were case studies, conference abstracts, unpublished data or grey literature. Additionally, studies conducted in chronic obstructive pulmonary disease or other respiratory conditions were excluded unless there were data on asthma that were considered relevant.
The opportunity
Smart inhalers offer comprehensive data on patient adherence and medication usage patterns, making these devices highly suitable for clinical trials and drug development. Although research demonstrating the impact of smart inhalers on clinically improved patient outcomes remains limited, especially for adults, their role in improving patient adherence is well documented across studies (Table 1).14,21–29 Audio–visual reminder feedback has had positive impacts on adherence in both adults and children compared with those who do not receive it.21 Using real-time and varied reminders minimizes the risk of ‘alert fatigue’ that can result from eventual habituation, which may occur with regular smart inhaler usage.21,22 These reminders are particularly beneficial for patients with lower levels of asthma adherence and control and may have a greater impact on younger generations who may be more accepting of digital technology.30 However, alongside these behavioural and population-based ideas, socioeconomic factors must also be considered. High costs, reliance on digital access and insurance limitations can restrict smart inhaler accessibility, particularly for lower-income and rural populations, affecting the overall implementation and uptake of these devices.14 Smart inhaler strategies need to consider these complex socioeconomic concerns and be multicomponent, reflecting the complex nature of populations and the multiple factors that influence adherence and non-adherence.15,22,30–32
Table 1: Overview of some key smart inhaler studies in asthma and findings21–26
| Study | Setting | Population | Duration | Type of smart inhaler | Intervention/control | Key findings | Other comments |
| Chan et al. (2015)22 | Auckland, New Zealand | Children | 6 months | SmartTrack inhaler (Adherium Ltd, Auckland, New Zealand [formerly Nexus6]) | Smart inhaler with audio–visual reminders enabled versus disabled | Children receiving the intervention (smart inhaler with ringtones) had better asthma control and adherence (84 versus 30%, p<0.0001) than the control group | No change in school attendance or unscheduled healthcare utilization |
| Foster et al. (2014)21 | Sydney, Australia | Individuals | 6 months | SmartTrack inhaler (Adherium Ltd, Auckland, New Zealand [formerly Nexus6]) | IRF and/or personalized adherence discussions compared with active usual care alone | Smart inhalers improved adherence (IRF group: 73 versus 46% in non-IRF group, p<0.0001) | Asthma control improved overall but no significant difference among groups |
| Morton et al. (2017)23 | Sheffield and Rotherham, UK | Children | 12 months | Smart inhaler and SmartTurbo (Adherium Ltd, Auckland, New Zealand) | Smart inhaler with reminder alarms, feedback, graphical adherence data for clinician and standard asthma care versus standard asthma care alone | Adherence was higher in the intervention group (70 versus 49%, p≤0.001) compared with the control | No significant difference in reported asthma control but intervention participants had fewer courses of oral steroids (p=0.008) and hospital admissions |
| Burgess et al. (2010)24 | Queensland, Australia | Children | 4 months | Smart inhaler (Adherium Ltd, Auckland, New Zealand [formerly Nexus6]) | Smart inhaler with patients told of adherence during review consultation versus nondisclosure to parents or treating physician | Adherence was significantly higher in the intervention group (79 versus 58%, p<0.01) | Small size of the study (26 children) so a larger study required for disease control implications |
| Mosnaim et al. (2024)25 | Illinois, USA | Individuals | 24 weeks | AirDuo Digihaler and ProAir Digihaler (Teva Pharmaceuticals, Tel Aviv, Israel) | Smart inhalers, app, Digital Health Platform and Dashboard versus standard of care (existing ICS/LABA and reliever inhalers) | Digital inhaler group had a higher odds of improved asthma control (mean odds ratio 1.35 [95% CI: 0.846–2.038]) | Digital inhaler group participants had more clinician–participant interactions compared with standard of care; this mostly addressed poor inhaler technique |
| Mosnaim et al. (2021)26 | Illinois, USA | Adults | 14 weeks | Propeller Health EMM and smartphone app | Smart inhalers with real-time usage monitoring, reminders and feedback through a smartphone app and clinician phone calls; control group had no feedback | SABA-free days increased significantly in the intervention versus control group (19 versus 6%), p=0.04 | ICS adherence stable in intervention (2% reduction) compared to a decrease by 17% in control (p<0.01); this produced a 15% difference (95% CI: 4–25; p<0.01) |
app = application; CI = confidence interval; EMM = electronic medication monitoring; ICS = inhaled corticosteroids; IRF = inhaler reminders and feedback; LABA = long-acting beta-agonist; SABA = short-acting beta-agonist.
Another critical factor influencing the effectiveness of smart inhalers is how they are used as part of healthcare interactions. Smart inhalers can help mediate positive interactions between patients and HCPs, who play a key role in addressing intentional or perceptual issues of non-adherence and reinforcing positive behavioural change.23,24,32,33 The act of using a smart inhaler can, in itself, increase awareness of inhaler issues for both patients and healthcare providers. For example, smart inhalers can detect improper inhaler techniques and provide direct feedback on inhaler use, which can then be monitored by clinicians or patients to guide users towards better methods.34 When used in this way, smart inhalers can support patients to be more proactive in their self-management and support better education – an aspect of asthma care often considered suboptimal.35 By facilitating better symptom control and providing greater opportunities for self-management, these smart inhalers could provide greater healthcare engagement and empowerment for patients with asthma compared with regular therapy. HCPs themselves are the other side of the end-user coin. Health professionals play a large role in harnessing the smart inhaler’s potential; clinician use and acceptance of these devices are crucial for their integration into routine clinical practice.29 Stakeholders across asthma care settings tend to view digital inhaler technology favourably, citing potential benefits such as improved asthma control, potential use as discussion aids, enhanced monitoring, increased patient involvement and more informed clinical decision-making.36 Real-time monitoring and alerts for worsening symptoms related to increased inhaler usage have also been reported to be features of particular appeal.36
Patient views and opinions of smart inhalers are equally important to the success of smart inhalers in practice. Overall, these devices have received positive feedback from patients, who highlight usability and implementation feasibility as specific advantages.37 There have also been associations with positive patient-reported outcomes, with general improvements noted through the use of smart inhalers in both childhood and adult asthma populations.16 In some cases, these improvements were even present without active clinician monitoring, although active clinician involvement is still an important variable for overall effective asthma management.16 With an increasing move towards digital health technologies to support self-management in other long-term conditions, it is likely patient acceptance and uptake of smart inhalers will continue to increase. Importantly, many studies assessing the benefits of smart inhalers have used devices lacking newer, more advanced capabilities, such as the ability to measure peak inspiratory flow (PIF) and provide feedback on technique. Future advancements in smart inhaler technology may yield even greater improvements in patient outcomes as more comprehensive data and personalized feedback are generated. With increased use, the cost of devices may decrease, with recent modelling showing the long-term cost-effectiveness of digital inhalers in managing difficult-to-treat asthma. This cost-effectiveness is a product of potential reductions in healthcare costs due to better disease management, fewer acute care admissions and decreased need for add-on biological prescriptions.38
Challenges
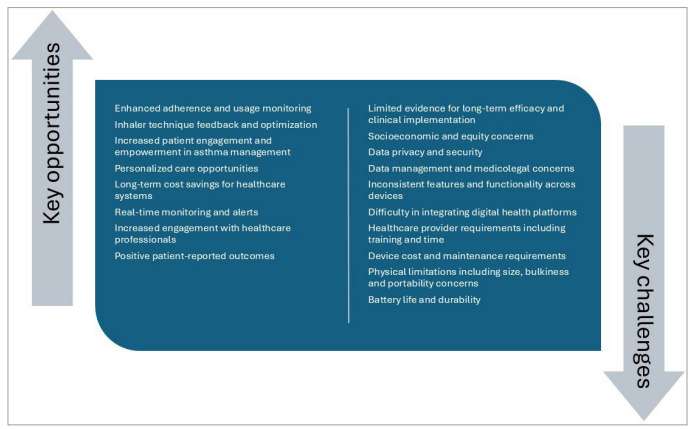
Smart inhalers offer many promising features, but their use remains mostly limited to clinical research settings. There is minimal use by health professionals in routine clinical care, and despite the availability of smart inhalers since the early 1980s, the concept of smart inhalers is still considered novel among patients and HCPs.39 From the clinician’s perspective, major barriers to clinical implementation include uncertainty in data handling and a lack of sustained evidence for efficacy (Figure 1).36 The lack of clinical uptake remains an issue despite growing evidence in this space.14 Whilst many trials show improvements in adherence, the mixed-/low-certainty data from the Cochrane review highlight the need for better-designed clinical studies that can address questions related to long-term effects on adherence (beyond the usual 6-month trial duration), patient acceptability, cost-effectiveness and effects on clinical outcomes such as exacerbations.14,40 For these devices to integrate smoothly into existing EHRs, they require compatibility with open platform systems or existing health systems that prevent the need for multiple portals per device.20,27 Furthermore, it remains unclear who is responsible for downloading, processing, interpreting and communicating the collected data to patients.36 Comparisons have been drawn to digital glucose monitoring, which, while offering significant benefits for diabetes management, has also been said to have introduced an increased workload and more responsibilities than expected for healthcare providers.41,42 Issues related to insurance coverage and reimbursement for both devices and associated visits have further complicated its integration into routine care, factors that have also been discussed in relation to smart inhalers.41
Figure 1: Opportunities and key challenges for smart inhaler use in clinical care
The short-term nature of research studies and selection bias, lack of blinding, high dropout rates and high heterogeneity across studies can make it difficult to see where the benefits of smart inhalers lie beyond adherence.17 Comparing smart inhalers with regular therapy is further complicated by behaviour changes related to data collection. As described by the Hawthorne effect, patients enrolled in clinical trials are more likely to adhere to proper inhaler techniques when aware of being observed. This phenomenon can distort study findings and reduce the generalizability of data to broader patient populations.25 This can impact both treatment arms, reducing the apparent efficacy of smart inhalers compared with the control group.25 Nevertheless, the behaviour change seen with smart inhalers is normally favourable, with positive consequences such as increased adherence, and in some cases, this occurs even without health professional intervention.26
There are also concerns relating to data management, which remains a critical issue among end users and is not isolated to smart inhaler technology alone.43 Patients have also expressed concerns about commercial interests driving the development of smart inhalers, particularly when sold online. Mitigating this requires clarity on any data ownership, access and storage management. Those using smart inhalers want to understand who can access their data and ensure it is securely managed. There are also worries from patients and the public about privacy breaches related to data storage and ‘Big Brother’ style surveillance, as well as fears of device damage, despite generally positive opinions and ease of use.28,44 To build trust among users, privacy, security and even ethical issues need to be well addressed. When done correctly, sharing data can be valuable, facilitating better medication use and improving inhalation techniques.20 The data collected by digital inhalers are also typically specific to the device, including the time and date of each dose, with some also logging personal metrics such as PIF. Location data are only gathered when paired with an app, and audio-based devices avoid capturing ambient sound by recording for typically less than a minute. If patients are concerned, users have the option to opt out of cloud sharing and instead transfer data directly from the device to a computer when needed. Some concerns may also be eased through knowledge of requirements for any cloud-transferred data to comply with the Health Insurance Portability and Accountability Act regulations.16 Given data concerns, if the purpose of data collection, access protocols and storage details are transparent from developers to patients, this area of concern can be mitigated. Part of supporting the successful implementation of smart inhalers is identifying the patients for whom the benefits of smart inhalers will outweigh the concerns. Ultimately, these patients are the target audience for these systems. Current studies, such as the Netherlands-based ACCEPTANCE trial (registration number: NL7854), aim to identify subgroups who might benefit most from smart inhaler therapy based on patient characteristics.45
Whilst identifying subgroups could be useful for personalizing therapy to those who need it most, considerations must be made to ensure this does not exacerbate inequities. Currently, digital health technologies face limitations related to access, skills or trust among specific populations, including but not limited to Black, Indigenous, People of Colour, the elderly, rural communities and individuals of lower socioeconomic status.46 Considerations regarding how smart inhalers may affect health disparities are key, as these devices may be less accessible to the patient groups who are most likely to require and benefit from their utilization.28,47,48 Smart inhaler self-management programs will need to incorporate methods to ensure inclusivity and equitable implementation and utilization.20 Examples could include the use of interfaces with different languages, icons or symbols that are culturally appropriate and age-appropriate design features. Factors such as the size and bulkiness of these devices, and the fact that multiple inhalers may each need different smart inhaler devices if not integrated into the inhaler device, can hinder their acceptance among some patient groups.36 Attaching specific sensors and smart elements to inhalers that are not designed for them can be problematic, and standardization of design will be vital for increasing uptake and enabling reliable comparison between devices.49 Historically, smart inhalers were add-on devices that were attached to traditional inhalers, but recent technological advancements have integrated electronic sensors directly into specific inhaler devices.50 The first smart inhaler with inbuilt monitoring capability was approved by the Food and Drug Administration in 2019 – the TEVA albuterol sulfate ProAir Digihaler (Teva Pharmaceuticals, Israel) – although the company recently announced the discontinuation of this product.51,52 The availability of in-built smart inhaler monitoring into pharmaceutical inhalers represented a major advance, particularly to support the adoption of this technology as part of routine care. However, this issue of device availability and cost remains a significant hurdle with high technology costs and inadequate funding, coupled with the constantly changing inhaler device market, limiting the widespread adoption of this smart inhaler technology.28 Despite the cost-effectiveness of smart inhalers demonstrated in the long term through improvements in medication adherence, inhaler technique and reduced need for expensive add-on biological treatments, the technology, demand and the market for smart inhalers continue to evolve, affecting the price, validity and accessibility of these devices.38 Additionally, evaluating the performance of smart inhalers remains challenging due to the lack of standardized usability metrics.
Future directions
Given the unique functionalities and benefits of smart inhaler technology, it would be expected that the uptake of smart inhalers among patients and clinicians would improve over time, particularly as the use of other digital technologies increases and market dynamics evolve. However, with key smart inhaler companies such as Teva Digihaler and Propeller Health withdrawing from the global markets, the progress made to date in moving smart inhalers towards clinical use is likely to be stifled or reversed. The longevity and routine clinical use of these technologies in the future remain to be seen. The smart inhaler market offers unique advantages to support personalized care, which is expected to grow with the expansion of smart inhaler technology research, and an increased burden of respiratory conditions.53 However, with the limited implementation of these devices into practice, there is a genuine risk of a reduction in the range of technologies available if investment in this sector reduces. Early co-creation with end-users, including policymakers and funders, in the development and design processes of these devices may mitigate this risk and enhance the clinical usage of these tools.54,55 HCPs are key stakeholders in the development process to achieve intuitive and straightforward software and devices. If not done correctly, this may hinder uptake in already time-constrained clinician–patient healthcare consultations.36 As a component of digital health technology, smart inhalers have the added potential to be incorporated into wider and more comprehensive health monitoring ecosystems. Constantly evolving artificial intelligence (AI) technology is already being used to predict future asthma exacerbations. In other respiratory conditions, leveraging AI for targeted drug delivery to specific areas of the lung is being studied.56,57 If smart inhalers can be incorporated into these digital ecosystems, there could be greater potential for uptake in clinical care. However, liability concerns for HCPs and institutions need to be addressed, especially when alerts could demand time-sensitive clinical action. While e-consents have been raised to help mitigate these from a manufacturer’s perspective, developing site-specific patient information will be necessary to explain how these systems work and outline expectations for patients.58
The integration of new technology and data handling in clinical care is inherently complex. This complexity arises from various elements, including medicolegal concerns, time, training, standardized data interpretation procedures and reimbursement schemes, all of which must be addressed for successful clinical implementation.29 To fully realize the potential of smart inhaler devices in both research and clinical settings, researchers, policymakers, pharmaceutical stakeholders and clinicians must work with device manufacturers to establish a roadmap that removes the barriers to implementation and generates the necessary effective evidence and start–stop criteria for using these devices in practice.20 More data on the target audiences that will benefit most from smart inhaler use, the effect on inequities and pragmatic funding or subsidy models are priority areas for future research. Understanding the temporal relationship between changes in adherence and their impact on outcomes, as well as their long-term sustainability, are key knowledge gaps that could be the subject of long-term, clinically focused studies.
Conclusion
Integrating smart inhalers into routine asthma care holds significant promise for improving personalized asthma management. These devices offer data and management capabilities that can be harnessed to enhance patient adherence, achieve precision medicine and create holistic, integrated approaches to predict future asthma attacks. Current limitations, such as practical usability, privacy concerns, reimbursement models and equitable access, remain barriers to the widespread adoption of smart inhalers. With these concerns addressed, smart inhalers may empower patients and clinicians alike, leading to better management of asthma and ultimately improved patient outcomes. This improvement is the ultimate goal of smart inhaler use, but collecting evidence to support this can be challenging in current research designs. As the technology develops, with greater innovation, collaboration among stakeholders and clarity regarding the finer details of implementation, the full potential of smart inhalers in clinical care can be realized within the expanding world of digital healthcare.17 If successfully implemented, smart inhalers could play a significant role in the needed improvement and personalization of asthma care.