Asthma is a common condition in childhood. Although significant advances have been made in the understanding of asthma in adults, many gaps in knowledge of the pathophysiology, prevention and management of childhood asthma remain.
Over the last several years, through analysis of the clinical, cellular and molecular characteristics of patients, it has become progressively clear that asthma is not a single disease, but rather a disorder with huge heterogeneity in pathogenesis, severity and treatment response. As a consequence of this holistic approach, the concepts of phenotype and endotype have become increasingly important, both in the research and clinical setting.1Dissecting sub-phenotypes of asthma could contribute to a greater knowledge of pathophysiology and natural history of the disease, and to more appropriate selection of treatment. For these reasons, the Unbiased BIOmarkers in PREDiction of respiratory disease outcomes (U-BIOPRED) project was set up to take advantage of the combination of extensive clinical characterisation and biological fingerprinting by ‘omics’ technologies for unbiased discovery of asthma phenotypes.2
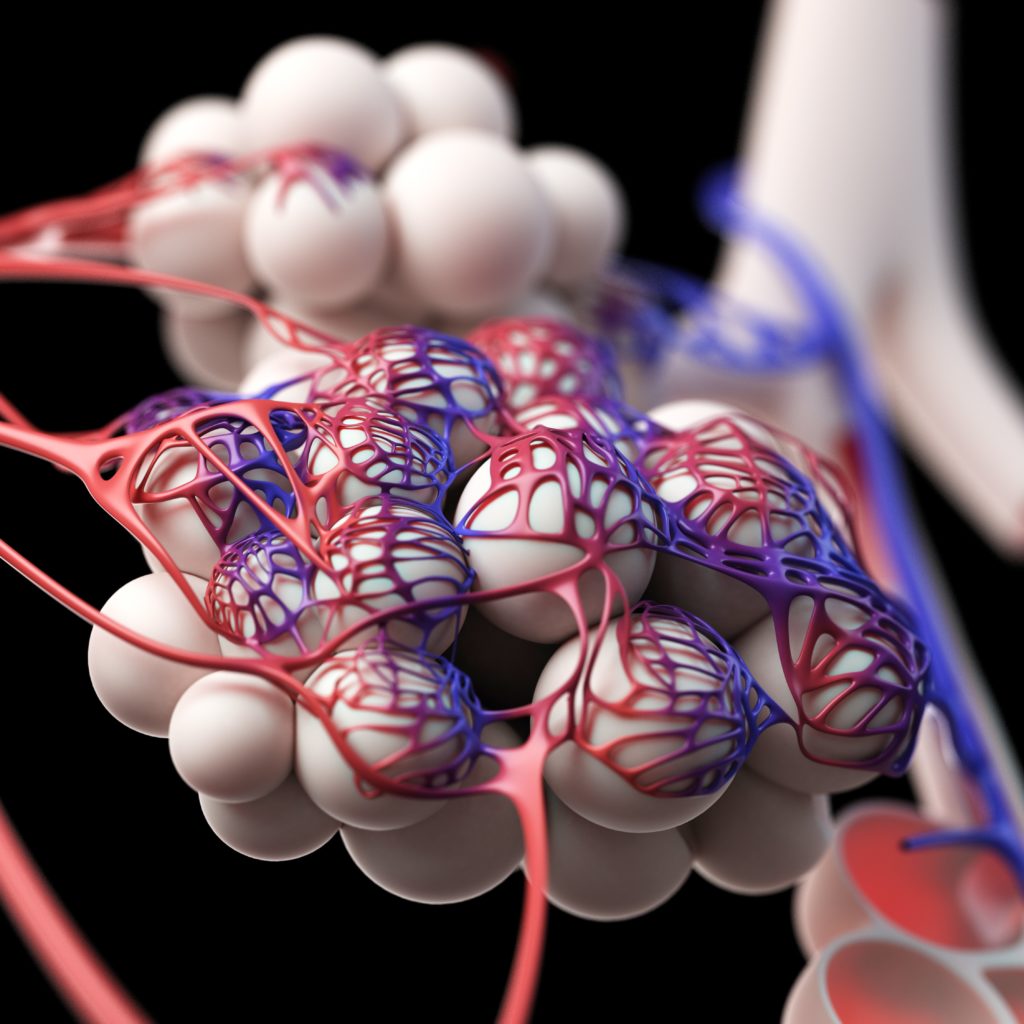
Asthma results from the interaction between the host’s genetics and the environment. Early allergic sensitisation and respiratory viral infections have been recognised as important risk factors for persistent wheezing and asthma development.3,4However, other factors such as exposure to air pollution and maternal stress in the prenatal and early postnatal period appear to influence the inception of asthma.5,6The relative contribution of each of these factors in influencing the inflammatory response of airway and asthma development is an unresolved question that calls for proper research in the field.
There is an increased awareness that specific microbial exposures can modulate lung immunity and development of pulmonary disease. Indeed, children with asthma by the time they are school age exhibit an aberrant immune response to pathogenic bacteria colonising the airways in early life.7It was also shown, by analysing serial bacterial pyrosequencing of the nasopharynx in young healthy children, that early patterns abundant in Haemophilus or Streptococcus were associated with more frequent upper respiratory tract infections.8These insights led to consideration of the potential relationship between bacterial microbiome and asthma as a new area of research. Furthermore, concomitant exposure to high levels of certain allergens and bacteria in early life has been shown to be beneficial in reducing allergic sensitisation and recurrent wheeze, suggesting new preventive strategies for wheezing and allergic diseases.9
Asthma exacerbations are common in childhood, especially in preschool years; they are responsible for significant morbidity and may have an influence on the future health of children. Recent studies suggest that exacerbations can lead to progressive loss of lung function.10Although the definition of what really constitutes an exacerbation is not clear, the relative importance of the number and severity of exacerbations in the natural history of asthma is still unknown. In asthmatic children, risk factors for exacerbation vary by season, thus information on individual patients might be beneficial in defining effective strategies to reduce the risk of these events.11If studies on prevention of exacerbations are properly addressed in the coming years, reduction in asthma morbidity is expected.
Despite substantial advances in identifying biological determinants of asthma, the role of inflammatory biomarkers in diagnosis, prediction of disease progression and treatment has remained elusive, given the heterogeneity of asthma and the presence of confounding factors. Further work is therefore needed to understand the potential clinical utility of biomarkers in asthma. Genetic and epigenetic markers might be useful in identifying response to therapy, and may represent a step towards a personalised approach. Rare β2-adrenergic receptor gene variants confer risk for severe asthma exacerbations in patients receiving long-acting β-agonist (LABA) therapy.12On the other hand, inhaled corticosteroids (ICS) have been shown to modulate the effect on bronchodilator response with variants in a specific gene among adults and children with asthma.13As treatment response to the main asthma therapies is partly genetically determined, pharmacogenetics may clear the way for the development of personalised medicine in children with asthma.
Consistent progression in asthma therapeutics has been obtained over the last decades. Several patient characteristics, lung function parameters and biomarkers have been shown to be useful in predicting treatment response or successful reduction of asthma medication, however, further information is needed in this area. It has recently been shown that, in the step-up treatment of asthma, addition of LABA is the preferred therapy in children without eczema, while those with eczema may respond better to increased ICS dose or leukotriene receptor antagonists step-up, depending on their race/ethnicity.14If validated, these novel findings might provide a personalised approach to targeting interventions based on specific and easily obtainable clinical features in children with uncontrolled asthma.
Another important necessity in the treatment of childhood asthma is to identify agents that exert preventing or disease-modifying effects, and to develop specific approaches to alter progression in children with established disease. Recent scientific research has focused on the study of new immunomodulators addressing specific pathways in asthma. Considerable experience has been gained with the clinical use of omalizumab, but ongoing research is urgently needed to better define optimal duration of therapy, to accurately predict the response to treatment, and to evaluate efficacy in nonatopic asthma.15 The possibility that omalizumab could prevent the development or modify the course of asthma when administered in early childhood to high-risk infants is another hypothesis to verify in future studies. There are several new medications on the horizon, including a number in the biologic modifier category, and perhaps one or a combination of these treatments may result in the effective prevention of onset and progression of asthma.
The path to greater knowledge of asthma is challenging and several issues remain unresolved. Personalised medicine for children with asthma aims to provide a tailored management of asthma, which will lead to faster and better asthma control, fewer adverse events and potential cost savings.16New and proper clinical trials are urgently needed to answer the many questions about the prevention, control and management of asthma that still remain open.