Nontuberculous mycobacteria (NTM) are a diverse group of bacteria with a wide spectrum of virulence.1 They are a microaerobic, non-motile organisms that have a lipid-rich, hydrophobic cell wall that is substantially thicker compared with most other bacteria.2 NTM are associated with biofilm formation, which contributes to disinfectant- and antibiotic-resistance.3–5 Many of these organisms are also resistant to high temperature and low pH.6–8 Ubiquitous in the environment, NTM are found with the greatest concentrations in water sources, both natural and treated, and in soil sources.9 There are currently over 170 species of mycobacteria and more are likely to be discovered in the future owing to improved culturing techniques and molecular technology advances.10
The majority of NTM-pulmonary disease (NTM-PD) infections are caused by the slow growing Mycobacterium avium complex (MAC) that includes Mycobacterium avium and Mycobacterium intracellulare, although other species including M. abscessus, M. xenopi, M. malmoense and M. kansasii can also cause lung disease. Not all NTM are considered pathogenic, with species such as Mycobacterium gordonae commonly isolated but not usually associated with the development of NTM-PD and a wide variability reported in the clinical relevance of species.12 Co-infection with different NTM strains or other bacteria has also been reported.9,13 NTM lung disease is characterised by clinical, microbiological and radiological criteria.1 High resolution computed tomography (CT) scanning may consist of a variety of disease patterns including nodular/bronchiectatic disease, fibrocavitary disease, solitary pulmonary nodule, disseminated disease, and hypersensitivity-like disease.1 Acquisition of NTM is believed to be from the environment; however, emerging literature, using sequencing of NTM isolates, suggest that indirect cross infection of M. abscessus is possible in patients with cystic fibrosis.14 This has led to changes in infection control standards in these patient groups.15,16
NTM are treated with antimicrobial chemotherapy, however treatment response is often poor, and side effects significant. Deciding which mycobacteria and patients to treat, and when, and the assessment of response to treatment is very difficult. The purpose of this review is to provide a succinct summary of issues surrounding the epidemiology, diagnosis and treatment of NTM-PD.
Epidemiology
In contrast to tuberculosis, NTM isolation in pulmonary specimens does not necessarily equate with active pulmonary disease, thus the incidence and prevalence of NTM pulmonary infections is difficult to characterise accurately.9 In addition, unlike tuberculosis, isolating NTM does not constitute a reportable condition in many countries. Population-based data for prevalence are available mainly from the US, Europe, New Zealand and Australia (where NTM isolation is reportable).17 These estimates are based on a mixture of microbiology laboratory reports, medical insurance returns and surveys. Annual prevalence estimates in North America and Australia range from 3.2 to 9.8 per 100,000.17 In Europe the estimates are generally lower, up to 3.3/100,000.17,18 The prevalence is significantly higher in certain regions and patient groups and period prevalence has been put at over 100/100,000 in the over 65-year-olds in the US over an 11-year period.19 The incidence of NTM disease is increasing throughout the world,11,17 with some estimates of an increase of 8.2% per year19 NTM-PD is currently more common in the US than tuberculosis.20 Improvements in awareness and diagnosis may in part underlie this rise.
In addition to the difference in prevalence, the predominant NTM species has also been reported to differ substantially by geographical region.21 To obtain information of NTM species distribution, in an NTM-Network European Trials Group (NET) collaborative study, species identification data for 20,182 patients, from 62 laboratories in 30 countries across six continents was collected.22 In total, 91 different species were isolated; M. avium complex predominated in most areas, although M. Kansaii predominated in Poland and Slovakia and M. Xenopi predominated in Hungary. MAC was most frequently isolated in Japan, Australia and South Africa.19,23–25
Pre-existing chronic lung disease (bronchiectasis, cystic fibrosis, chronic obstructive pulmonary disease [COPD], idiopathic pulmonary fibrosis) predisposes patients to acquiring NTM respiratory infection.26,27 Other disease risk factors include thoracic skeletal abnormalities, taking immunomodulatory drugs and rheumatoid arthritis.17 Clustering of disease within families may suggest a heritable genetic predisposition to susceptibility of NTM-PD. Defects in interleukin-12 and interferon-gamma defence pathways may increase susceptibility to NTM infections28 and these defects have been described both in individuals and in familial clustering of disease.29 A recent study utilising exome sequencing of patients, family members and controls has suggested a multihit, multi-genetic predisposition to NTM disease.30 In addition to host predisposition, environmental exposure is likely to play a significant role in predisposition to NTM-PD, as suggested by variance in prevalence and mortality between and within countries. In studies in the US,19 Japan31 and Australia,32 temperature, humidity and alteration in soil components have impacted on NTM prevalence.
Mortality in NTM-PD is significant, with 5-year mortality after definite NTM disease at 40.1%, according to Danish population data.33 In this study, patients with M. xenopi had the worst prognosis. A randomised controlled study of NTM treatment regimens by the British Thoracic Society demonstrated similarly high 5-year all-cause mortality rates of 38.8% for MAC, 48.5% for M. malmoense and 38.2% for M. xenopi.34Other retrospective studies have specifically looked at MAC lung disease and assessed specific characteristics associated with a worse prognosis. The 5-year all-cause mortality of patients with definite pulmonary MAC was 25.6% in a retrospective study (n=164) of patients with pulmonary MAC disease.35,36 High Charlson comorbidity index scores and the presence of cavitary lesions were associated with higher mortality. Prognostic factors of allcause mortality were identified in a retrospective analysis of 634 HIV-negative patients with MAC lung disease.37 The all-cause 5-year mortality was 23.9% and negative prognostic factors of all-cause mortality included: male sex, older age, presence of comorbidity, body mass index (BMI) <18.5 kg/m2, anaemia, hypoalbuminemia and erythrocyte sedimentation rate ≥50 mm/h. In a retrospective review of 72 patients with nodular bronchiectatic MAC lung disease, lower BMI, cavities and macrolide-resistance at initial visit seemed to be

associated with progression to deteriorating disease over 5 years.38 In another retrospective analysis, which involved data from 52 adults with non cystic fibrosis bronchiectasis and coexisting MAC infection over a 5-year period, chronic pulmonary aspergillosis and nodules with cavitation and emphysema on high-resolution CT scans at presentation were identified as a strong independent predictors of mortality.39 In a retrospective cohort study of 124 patients with NTM, predominately M. avium, the most important predictor for increased mortality was the radiological appearance of a consolidation.40 Direct comparisons between studies are difficult due to the differences in treatment regimens, patient cohorts and methodologies.
Diagnosis
NTM are ubiquitous in the environment and isolation from sputum does not always signify disease. The American Thoracic Society (ATS) and the Infectious Disease Society of American (IDSA) jointly published guidelines on diagnosis of NTM infections in 2007 (Table 1).1 An early differential diagnosis of NTM lung disease from pulmonary tuberculousis is important because the therapeutic regimen differs from that of pulmonary tuberculousis and it is not necessary to track the contacts of patients with NTM-PD.41
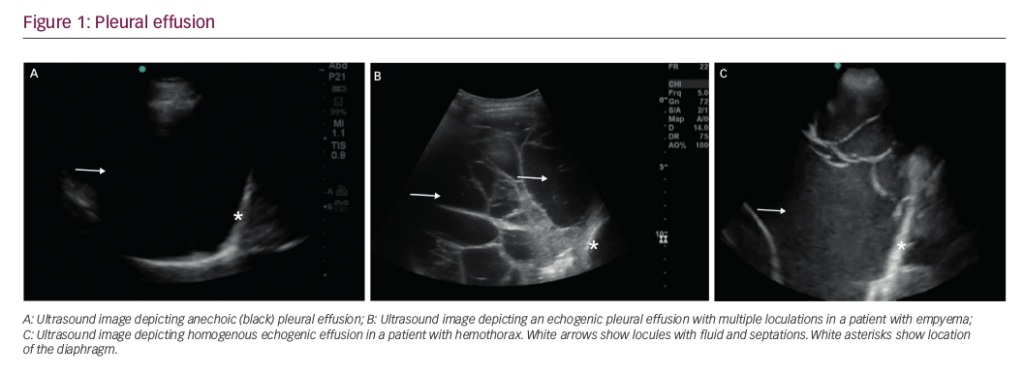
Symptoms are variable although chronic cough with or without sputum production or haemoptysis, is common. Other symptoms include fatigue, malaise, dyspnoea, fever, chest pain and weight loss. The evaluation of NTMs is often complicated by coexisting lung diseases including cystic fibrosis, bronchiectasis and pneumoconiosis. For patients in whom diagnosis is not clear, expert consultation should be sought. High resolution CT scans showing NTM-PD are presented in Figure 1.

Treatment
The 2007 ATS/IDSA guidelines are the most commonly followed worldwide. They recommend that treatment for most patients with nodular/bronchiectatic MAC disease involves a three-times-weekly regimen of clarithromycin (1,000 mg) or azithromycin (500 mg), rifampin (600 mg) and ethambutol (25 mg/kg), although in many cases daily treatment may be appropriate.42 For patients with fibrocavitary MAC lung disease or severe nodular/bronchiectatic disease, a daily regimen of clarithromycin (1,000 mg) or azithromycin (250 mg), rifampin (600 mg) or rifabutin (150–300 mg) and ethambutol (15 mg/kg) with consideration of three-times-weekly amikacin or streptomycin early in therapy is recommended. Patients should be treated until culture negative for 1 year while receiving antibacterial therapy.1 Similar combinations of drugs have also been suggested for other NTM that commonly cause NTM-PD such as M. kansasii, M. malmoense and M. xenopi.1 No established regimens of proven efficacy exist for M. abscessus; although standard treatment based on case series consists of an induction phase of intravenous therapy including medications such as amikacin, carbapenem, tigecycline or cefoxitim, followed by a continuation phase of oral antibiotics.43 A macrolide-based regimen is often used and surgical debridement may also be important. However, macrolide resistance is common in M. abscessus because the organism possesses an inducible macrolide-resistance gene.44,45 In some instances more than one NTM species is present and there are no data available to guide the clinician in these cases so they need to be evaluated and treated on an individual basis.13
In some patients, clinical improvement and culture conversion will be the aim, however, for others, stability will be a more realistic target.1 The potential toxicity of anti-mycobacterial therapy must be


balanced against a sometimes indolent clinical course. A patient’s comorbidities and quality-of-life issues are also important to take into account. There are currently insufficient data on the natural history of untreated infections to guide clinical decision-making in this respect. In clinical practice it is often difficult to discern whether or not disease progression is due to NTM. Even if NTM is diagnosed, lung disease treatment may not always be needed. For patients with indolent NTM lung disease there is usually enough time for careful consideration of the optimal management. Once a risk-benefit decision has been made to begin NTM therapy, the choice of agents and duration of treatment is based on the specific organism and extent of disease. Before a decision is made to treat with the aim of improving symptoms such as cough, it should be considered whether the symptoms are attributable to a concomitant diagnoses of bronchiectasis, sinus disease and/or gastroesophageal reflux disease.
Limitations of current treatment
The drugs used for treatment of NTM have not been developed specifically for these infections but rather, the rationale for their use has often been extrapolated from the treatment of tuberculosis and are often based on personal experiences of the treating clinician. The long duration of treatment often leads to adverse drug reactions, increased potential for drug–drug interactions and nonadherence to treatment or treatment discontinuation.46 Typical adverse events of drugs used to treat NTM infections and drug–drug interactions are summarised in Tables 2 and 3. NTM infections are common in elderly people and age-related changes in drug absorption, metabolism and excretion may lead to a decline in efficacy and increased toxicity.47
Treatment practices
Adherence to the 2007 ATS/IDSA guidelines for the treatment of NTMPD in the US has been revealed to be poor, with suboptimal antibiotic regimens commonly prescribed across physician specialities.48 Overall, 95% of the 1,286 physicians selected were in the following specialties: pulmonology, infectious diseases (IDs), internal medicine or family/ general practice. Out of 349 physicians who completed questionnaires, only 13% of antibiotic regimens prescribed for patients with MAC, were in accordance to ATS/IDSA guidelines. Around half (56%) did not include a macrolide and 16% were for macrolide monotherapy.48
Conclusions and future perspectives
NTM-PD is increasing in prevalence, leading to an emerging public health problem.17,49 More work is needed to investigate species-specific environmental niches as causes of differences in global isolation patterns.22 Better management of the disease remains an unmet need with improvements required in diagnosis, treatment, patient adherence to treatment and patient outcome. Present treatment options are limited, with drug regimens associated with significant failure and intolerance. Individualised treatment should be administered after careful consideration of both the efficacy and risk of adverse events.
New treatments for NTM infections are imperative and more prospective studies are warranted to define suitable drug regimens for different NTM species and to better define the natural history and epidemiology of this condition. Due to the complexity of the problem, involvement of specialist centres is important.